Introduction
The COVID-19 pandemic has resulted in the widespread use of aerosol personal protective equipment (PPE) to prevent disease transmission in healthcare environments. Other forms of PPE are a heat stress1 and heat stress has a negative impact upon cognitive and motor function2,3. The use of aerosol PPE is reported subjectively to have a negative impact upon healthcare workers’ performance and wellbeing4, but the consequences have not been assessed objectively.
Aims
This study aimed to quantify the heat stress associated with aerosol PPE and to investigate its impact upon mood, cognitive and motor function, and task performance.
Methods
Ethical approval was obtained from Imperial College Research Ethics Committee (20IC6445). Sixteen healthy subjects (eight male) undertook an exercise protocol, which simulated the metabolic expenditure of hospital work5: once wearing aerosol PPE (PPE visit) and once wearing standard surgical attire (control visit). The order of the visits was randomised and they were scheduled approximately one week apart. Subjects walked on a treadmill for 2 hours followed by a 30-minute recovery period. Core temperature, heart rate, urine specific gravity, grip strength, mood state (Bond-Lader scales), executive function (One-Touch Stockings task) and task performance (Intubation of a Manikin) were recorded. Data are presented as mean (SD) and analysis performed with two-way repeated measures ANOVA.
Results
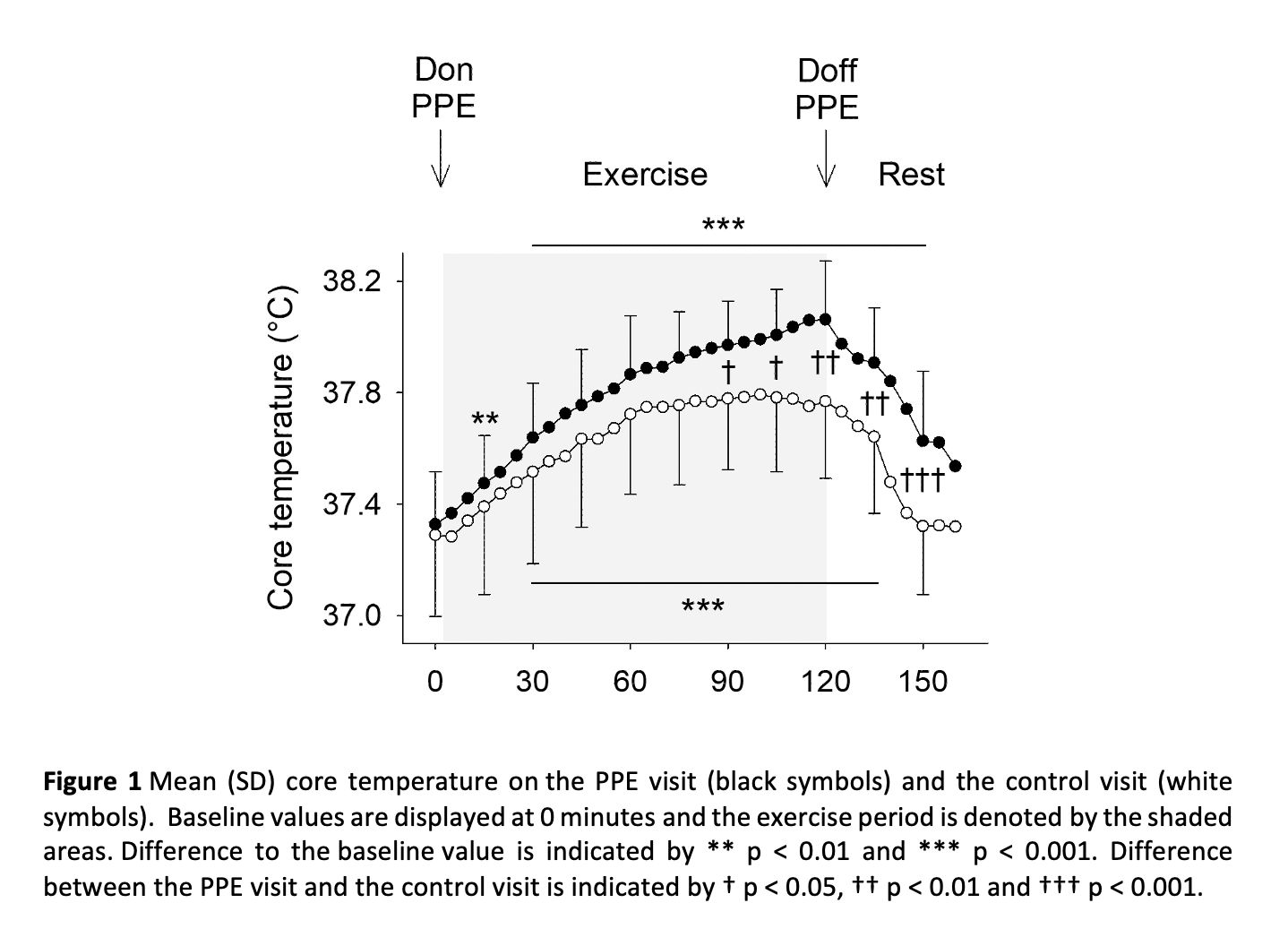
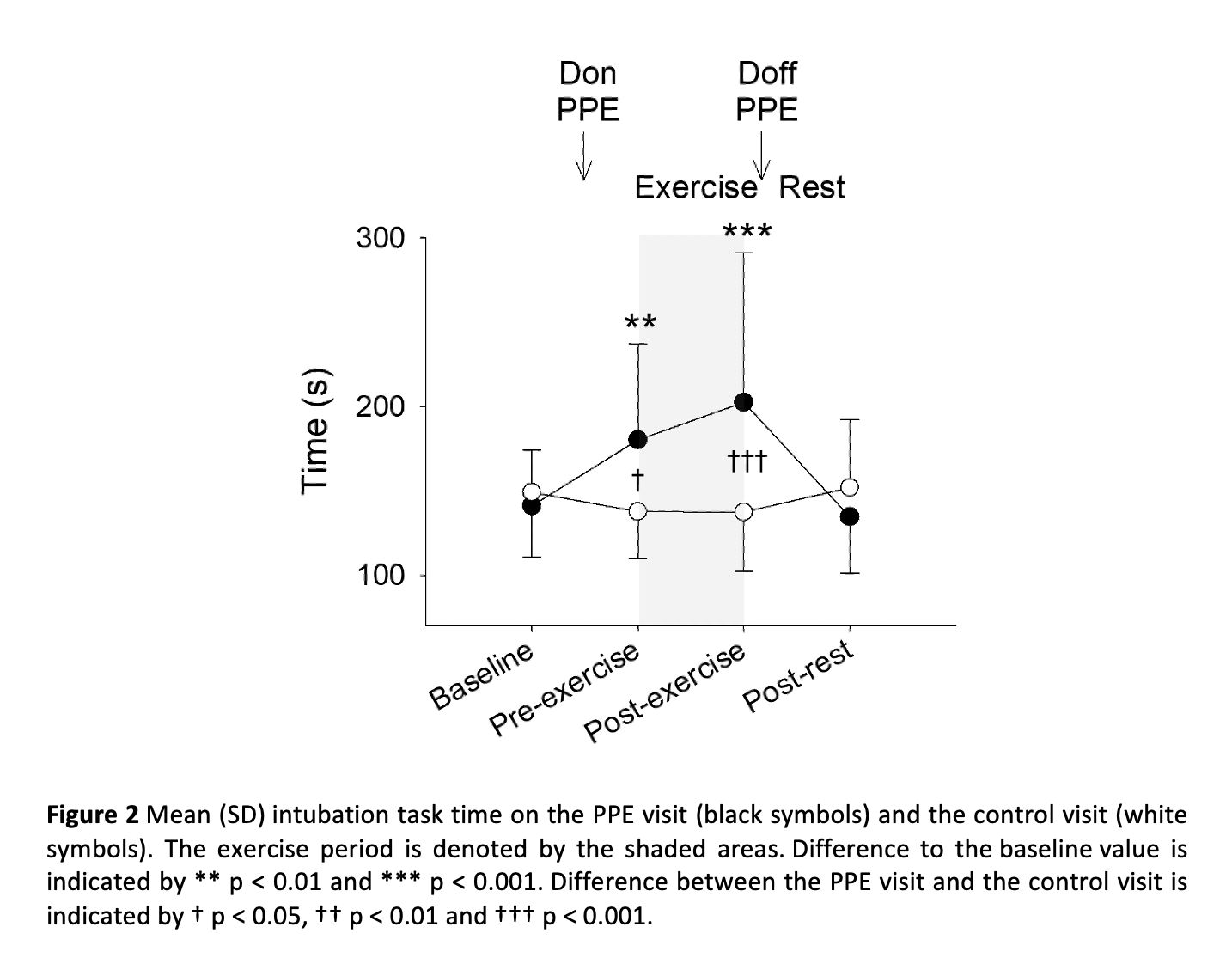
Core temperature was greater on the PPE visit than on the control visit from 90 minutes of exercise until the end of the rest period (p < 0.05, Figure 1). Maximum core temperature was 38.1 (0.2)°C on the PPE visit and 37.8 (0.3)°C on the control visit. Heart rate was greater on the PPE visit from 30 minutes of exercise until 15 minutes of the rest period (p < 0.01). Maximum heart rate was 121 (9) bpm on the PPE visit and 109 (9) bpm on the control visit. Urine specific gravity was greater following exercise on the PPE visit (1.023 (0.006)) than the control visit (1.019 (0.008), p = 0.04). Alertness (p < 0.001) and contentment (p < 0.001) were less following exercise on the PPE visit, but calmness did not differ between the visits (p = 0.24). One-Touch Stockings latency (p = 0.93) and accuracy (p = 0.19) did not differ between the visits. Grip strength was less on the PPE visit following exercise in the right (-4 (6) N) and left hands (-4 (4) N) compared to the control visit (p < 0.01). Time to complete the intubation task was greater on the PPE visit after donning PPE (+43 (66) s; p < 0.05) and after the exercise period (+65 (103) s; p < 0.01, Figure 2).
Conclusion
This study demonstrates that wearing aerosol PPE for 2 hours in a simulated hospital environment results in heat exhaustion and has a negative impact upon mood, motor function and task performance. Cognitive function was not affected, but this may be due to insufficient heat stress. Whilst wearing PPE is important to prevent disease transmission, strategies should be developed to limit its impact upon healthcare workers’ performance and wellbeing.
Biomedical Basis of Elite Performance 2022 (University of Nottingham, UK) (2022) Proc Physiol Soc 49, PC09
Poster Communications: Heat stress associated with aerosol personal protective equipment (PPE) and its impact on mood, cognitive and motor function: a randomised controlled cross-over study
Alexander John Wickham1, Alison Hazel McGregor1, Nishant Chaudhari2, Christopher John Mullington2,1, Paul Henry Strutton2
1 Theatres and Anaesthesia, Imperial College Healthcare NHS Trust 2 MSk Lab, Imperial College london
View other abstracts by:
Where applicable, experiments conform with Society ethical requirements.