Background: Cardiopulmonary exercise testing (CPET) is used to determine cardiorespiratory fitness (CRF) in patients prior to major surgery given its capacity to predict post-operative survival [1]. Low CRF is attributed to 17% of postoperative mortality, presents greater risk than traditional measures of cardiovascular disease, and unfit patients experience a 5-fold greater mortality hazard [2]. CPET is preferably conducted to the limit of tolerance and primary metrics include, anaerobic threshold (AT), peak oxygen consumption (V̇O2 peak), and ventilatory equivalent for carbon dioxide at AT (V̇E/V̇CO2-AT) [3]. In non-surgical populations, musculoskeletal (MSK) conditions affect up to 1 in 3 people and are associated with a two-fold likelihood of being physically inactive [4]. In this study we observed a large cohort of patients who underwent CPET prior to colorectal surgery to identify the prevalence of MSK limitation. We then compared to what extent potential inability to provide authentic maximal CPET effort may inform metrics used for surgical risk stratification in this population.
Methods: A consecutive sample of 640 patients scheduled for elective colorectal surgery who attended CPET testing were retrospectively examined. CPET was conducted in accordance with consensus clinical guidelines [5] using cycle ergometry (Lode, Gronigen, The Netherlands) and a Medgraphics Ultima metabolic cart (MedGraphics™, Gloucester, UK). Patients exercised to their limit of tolerance to provide information for prognostic and diagnostic utility. The Medgraphics Breeze™ software automatically determined V̇O2 peak and respiratory exchange ratio (RER). The AT was manually interpreted using the V-slope method and V̇E/V̇CO2-AT calculated. Immediately following test termination patients were asked why they stopped, and responses used to stratify groups by prevalence of MSK pain (MSK+ or MSK-). Following confirmation of distribution normality (Shapiro W Wilks tests), data were analysed using independent samples t-tests for continuous data, or χ2 tests for frequency counts. Data are expressed as mean ± SD and significance established at P < 0.05.
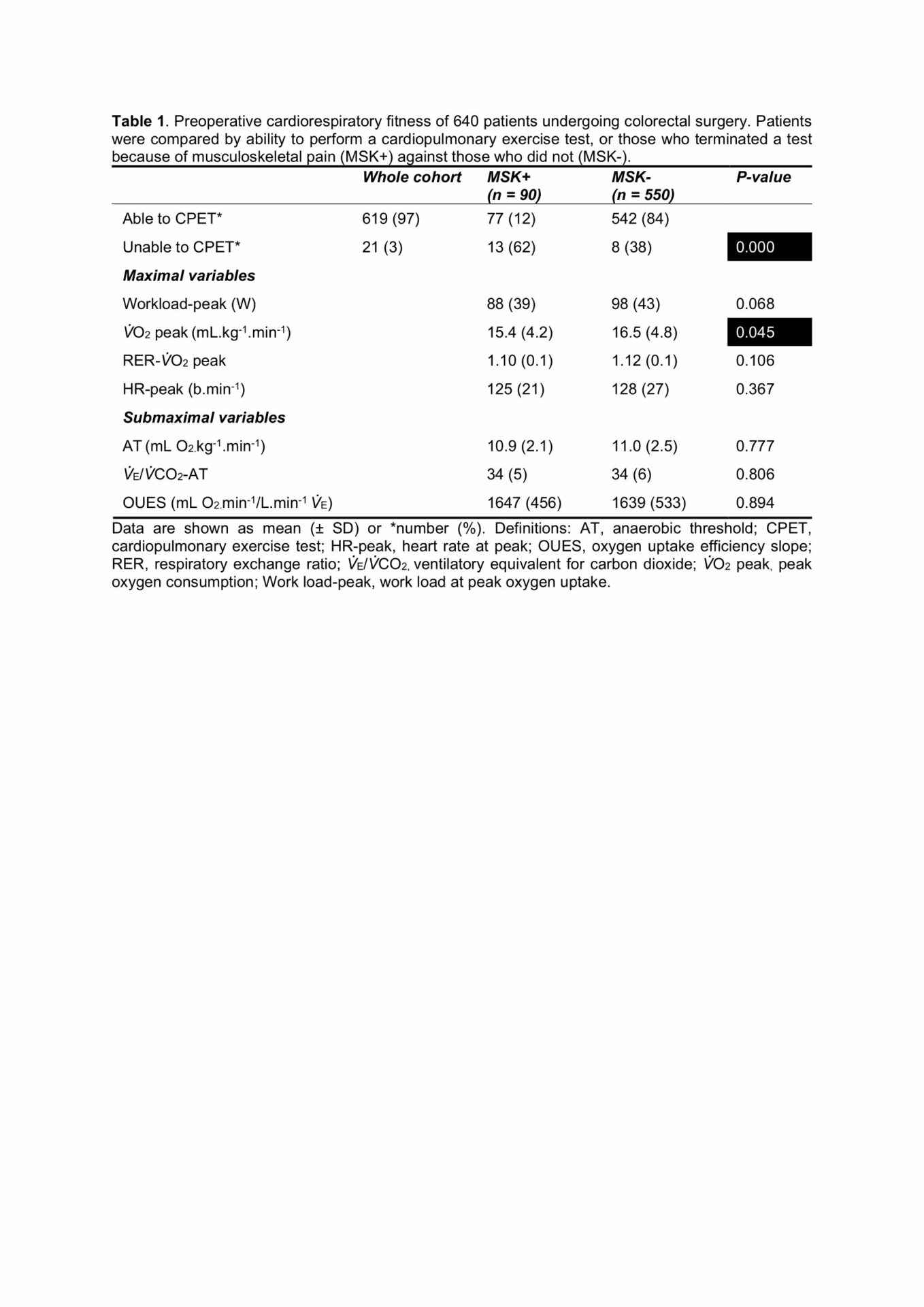
Results: Not all patients completed CPET. Seventy seven of 619 patients (12%) who completed CPET reported MSK pain as the reason for terminating prematurely, whilst 13 of the 21 (62%) patients unable to perform CPET were prevented in doing so by MSK limitations. Patients who reported MSK pain as the cause for premature test termination exhibited lower V̇O2 peak whereas the submaximal AT metrics were comparable (Table 1).
Conclusions: Exercise limitation due to MSK pain is prevalent in patients undergoing preoperative CPET. Patients unable to CPET have high risk of postoperative mortality and MSK limitation is often what prevents them from performing a test. Of MSK+ patients able to CPET, reduced V̇O2 peak is likely, and caution should be applied to this metric. Clinicians should consider metrics, such as the AT, that do not require maximal effort and investigate alternatives like the oxygen uptake efficiency slope allowing opportunity to account for disruption by early termination of exercise in these patients.