The use of cigarettes and e-cigarettes both increase blood pressure. Inspiratory muscle strength training (IMST) can lower blood pressure in healthy subjects (De Lucia et al, 2018). The aim of this study is to investigate whether IMST affects blood pressure and heart rate variability (HRV), a marker of cardiac autonomic function, in a group of smokers and non-smokers.
15 participants volunteered for this study (11 female). 5 participants smoked both cigarettes and e-cigarettes. Ethical approval was granted by the Science & Engineering Research Ethics committee, University of Plymouth, in accordance with the Declaration of Helsinki. All participants gave informed written consent. Participants completed a health questionnaire including information on exercise and smoking. Anthropometry, systolic blood pressure (SBP) and diastolic blood pressure (DBP) were initially recorded, along with respiratory muscle strength (RMS); using the mean of maximum inspiratory pressure (MIP) and maximum expiratory pressure (MEP). 50% of the MIP reading was used to determine the resistance on two different brands of IMST (Threshold and Breather devices). Subjects were seated and five, 1-minute experiments were conducted; 1-minute rest, 1-minute IMST Device 1, 1-minute rest 2, 1-minute IMST Device 2 and 1-minute rest 3. IMST device order was randomised. Blood pressure, oxygen saturation (SpO2), Borg scale for breathlessness, chest plethysmography and ECG were recorded for all experiments, with a nose-clip being worn. LabChart software and a PowerLab were used for data acquisition. HRV was analysed using time domain (heart rate – HR, standard deviation of the RR interval – SDRR), frequency domain (low and high frequency – LF and HF) and Poincaré analysis (SD1 and SD2). Repeated measures ANOVA (RMANOVA) and SPSS software was used to analyse the data (n=15). The probability of <0.05 was taken a statistically significant. Post-hoc analysis using pairwise comparisons between means was performed.
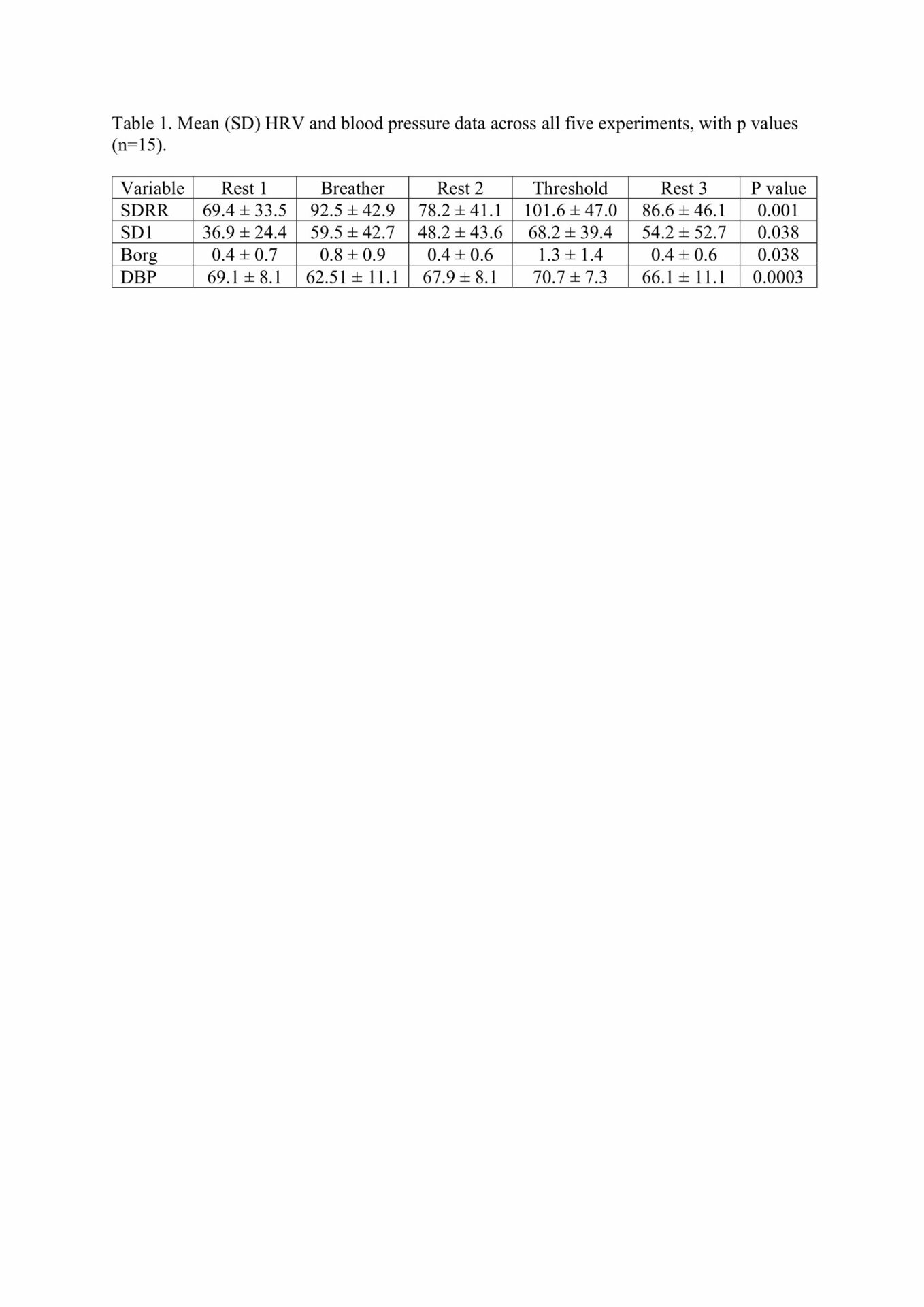
SDRR, SD1, Borg and DBP were all significantly different across all five interventions (Table 1). SDRR and SD1 were higher with both IMST devices, Borg was only higher with Device 2 (Threshold), while DBP fell with Device 1 (Breather). HR (p=0.45), LF (p=0.95), HF (p=0.96), SBP (p=0.12) and SpO2 (p=0.18) did not show any significant changes over the five interventions. No significant differences were noted between smokers (n=5) and non-smokers (n=10).
The main findings from this study are the IMST devices resulted in time domain HRV parameters, breathlessness and DBP to differ. Unlike the work of De Lucia et al. (2018), which showed a drop in both SBP and DBP, our study only showed a drop in DBP. Reasons for this difference could include the acute duration of IMST and the fact we used a lower percentage of MIP when giving IMST. A low statistical power was most likely the reason no difference in smokers was found in the current study.