Background: Functional brain imaging studies of dyspnoea consistently report activation of insular cortex (Evans et al., 2002; Banzett et al., 2000). The precise role and importance of the insula in dyspnoea perception cannot be discerned from brain imaging studies alone, alternative approaches are needed to establish a structure-function relationship. We had the opportunity to study patients with insular gliomas and hypothesised that sensitivity to experimentally induced air hunger would be diminished.
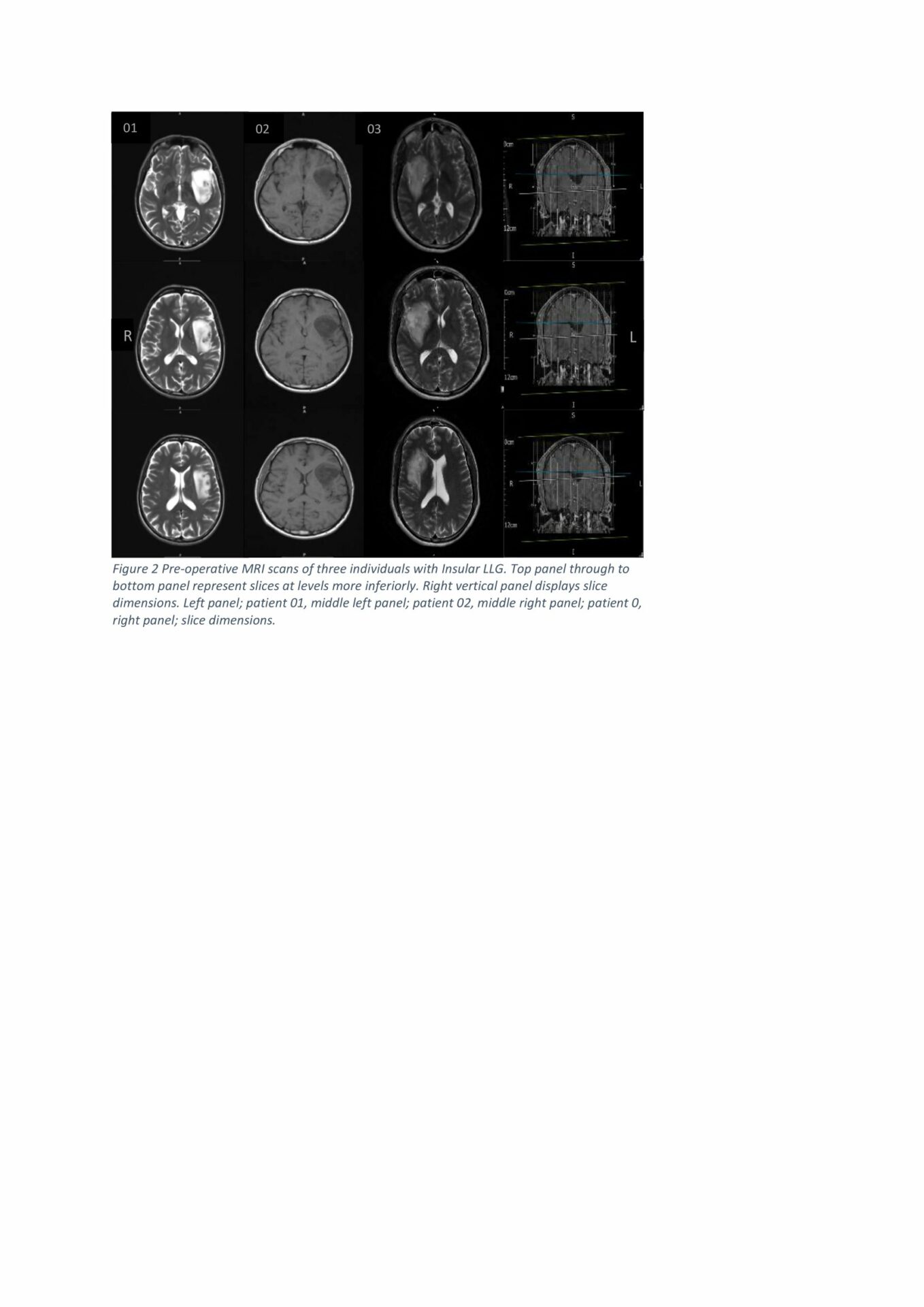
Method: Three patients with low grade insular glioma and three healthy age matched controls underwent incremental hypercapnic air hunger (AH) tests. This involved 1min increments of 1.3% in inspired CO2 raising end tidal PCO2 up to 55mmHg while ventilation was constrained to their baseline level (mean±sd 10.7±2.3 and 9.7±0.5 L/min in patients and controls, respectively). Participants rated their air hunger on a 10cm visual analogue scale (VAS) every 15 seconds throughout the test.
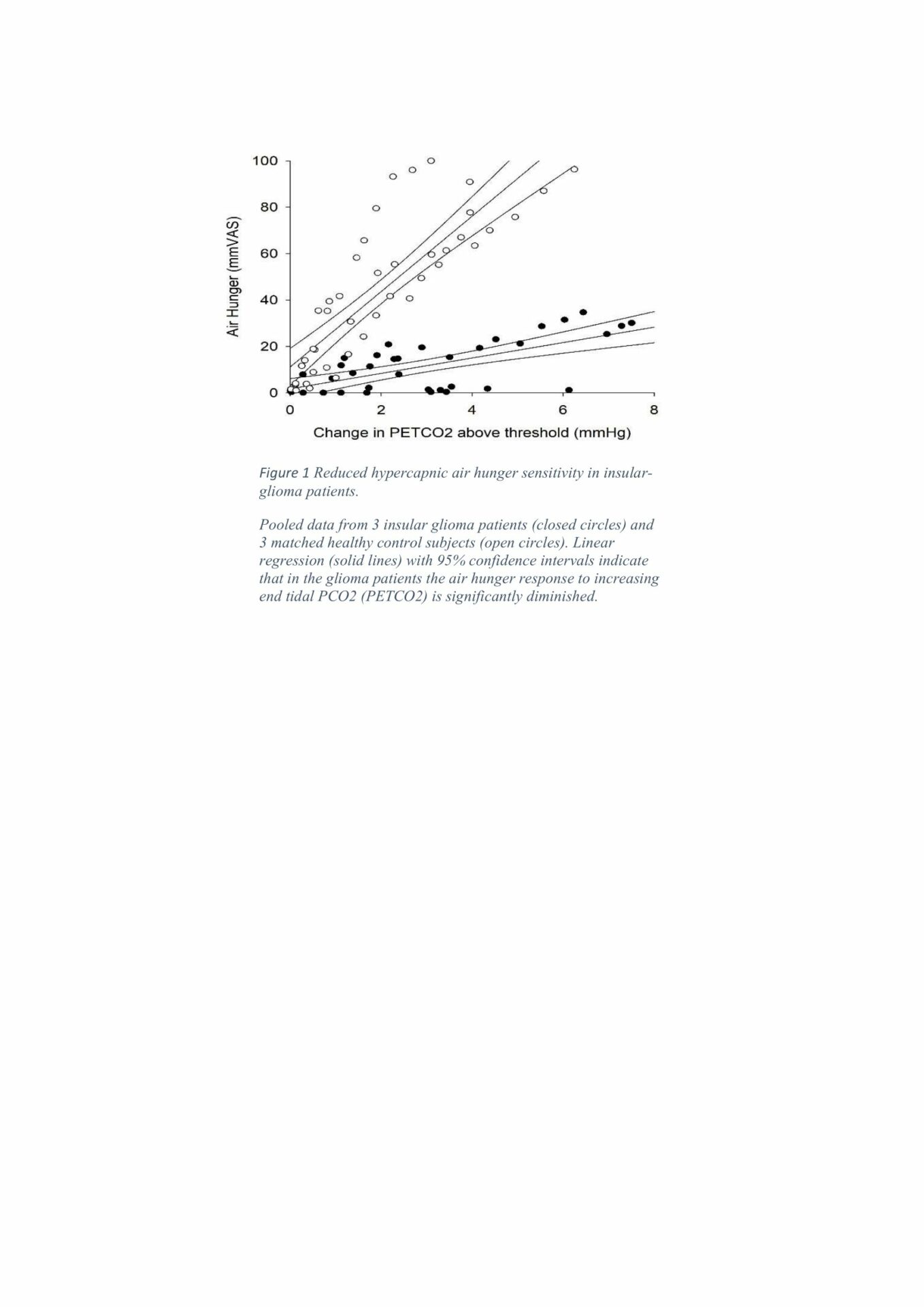
Results: The three glioma patients (aged 38-45 years, one female) produced a substantially lower hypercapnic air hunger stimulus response slope compared to age matched healthy controls (aged 34-41 years, one female); mean±sd slopes were 2.27±2.6 vs 23.1±11mmVAS/mmHg PCO2. This difference approached significance (p=0.08). The lowest slope in the healthy control group was 14.3mm/mmHg PCO2. The mean±sd AH threshold was the same for both patient and control group (43±4.5 versus 43±3.6mmHg PCO2 ). During debrief, patients comments suggested that it was specifically the affective component of breathlessness that was diminished. The one patient who has had surgery to remove the glioma continued to show a reduced sensitivity when re-tested post surgery( 6.7mm/mmHg) with a slight rightward shift in threshold for AH.
Conclusion: This data suggests that low grade insular glioma generates insensitivity to hypercapnic air hunger, particularly the affective component. If a fully powered study verifies these findings, this will add support for targeting this region for symptomatic relief of intractable dyspnoea in patients with incurable cardiopulmonary conditions.