Physiology News Magazine
Developing trusted healthcare tools: How physiology can unlock the potential of artificial intelligence for health
Membership
Developing trusted healthcare tools: How physiology can unlock the potential of artificial intelligence for health
Membership
https://doi.org/10.36866/pn.132.42
In June 2023, The Physiological Society launched its policy report, “From ‘Black Box’ to Trusted Healthcare Tools” in the Houses of Parliament. This report places a spotlight on the role of artificial intelligence (AI) in healthcare and the necessity of integrating physiological evidence into its application to prevent health inequalities.
The report was based on consultations with over 30 leading experts in the field. The evidence gathered and case studies developed highlight how physiological measurements and knowledge are being used to develop AI tools, as well as examine how to ensure the safe and effective implementation of AI to support clinical decision-making and transform healthcare.
On these pages we share with you a few of the case studies published in the report to showcase the human-centred technologies being developed to improve the quality of healthcare, from assessment to monitoring conditions and providing new treatments for patients.
AI as an everyday tool: optimising intravenous fluid and vasopressor doses in patients with sepsis in intensive care
Professor Aldo Faisal, Dr Matthieu Komorowski, Professor Anthony Gordon
Imperial College London, UK
Sepsis is a life-threatening condition, when the body’s response to severe infection causes vital organs to stop working normally and is a major worldwide healthcare challenge and the primary cause of death in hospitals. A key part of the treatment of sepsis is the administration of intravenous fluids and vasopressors to keep the cardiovascular system working while the antibiotics do their work. However, there is huge uncertainty and vast interpatient differences around the individual dosing of these two drugs in an individual patient. An AI tool to personalise these medications and their dosages could improve patient survival.
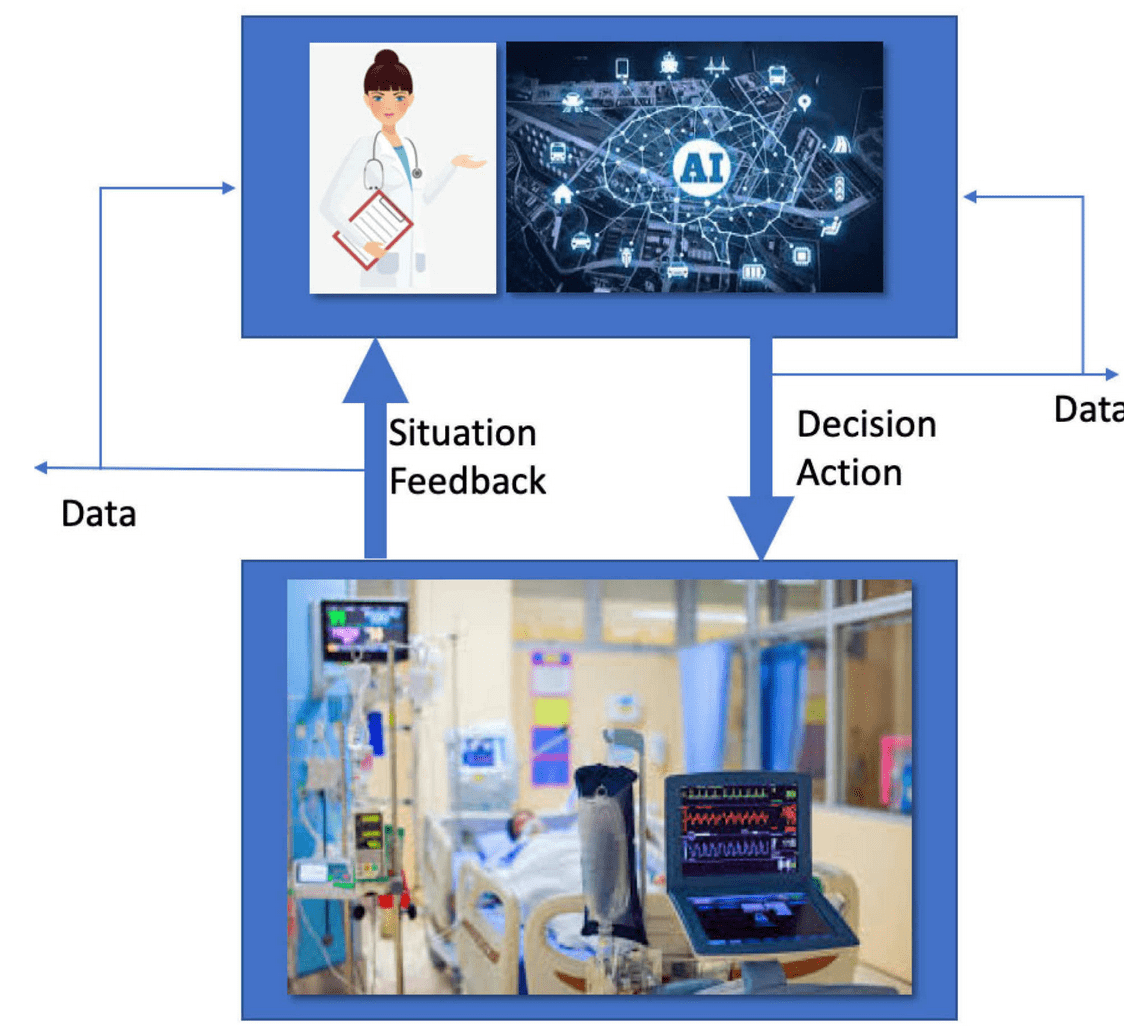
We have developed a new method to automatically and continuously review and recommend the best doses of these medications to clinicians. To this end we developed AI techniques applied to large medical databases, including large amounts of physiological data, that learn from patient data and doctors’ treatment decisions the best strategy for treatment. As previous work had shown potential to improve patient survival rates, our team at Imperial College London has been developing a tool capable of processing patient data within the electronic patient record of NHS hospitals in real time, to recommend a course of action. This tool is being evaluated and refined in simulation studies being deployed across four London hospitals.
The AI Clinician extracted implicit knowledge from an amount of patient data that exceeds by many-fold the life-time experience of human clinicians and learned optimal treatment by analysing myriad (often suboptimal) treatment decisions. Its use is now being systematically tested to see how it performs with NHS clinicians in both simulated and real clinical scenarios.
It has previously been demonstrated that the value of the AI Clinician’s selected treatment is on average reliably higher than that of human clinicians. It is currently being tested in four NHS hospitals, first in a “shadow mode” when the AI recommendation is not provided to the clinicians to allow comparison and understanding of actual decisions vs recommended AI decisions. In the second stage, that started this summer, the clinical evaluation is displayed at the bedside to the treating clinicians to allow researchers to assess the clinical acceptability of the tool and also confirm the technical feasibility for future large-scale clinical trials.
Understanding the basis of reproductive health through machine learning
Professor Rohan Lewis, University of Southampton, UK

By enabling babies to grow well in the womb, the health of both mother and the child can be improved. We are exploring structure and function relationships in the placenta and endometrium. Advances in imaging techniques are helping to achieve this, but they generate complex datasets, which are time-consuming to analyse. Using machine learning, our research seeks to analyse these images more quickly and to gain additional insights from this technology.
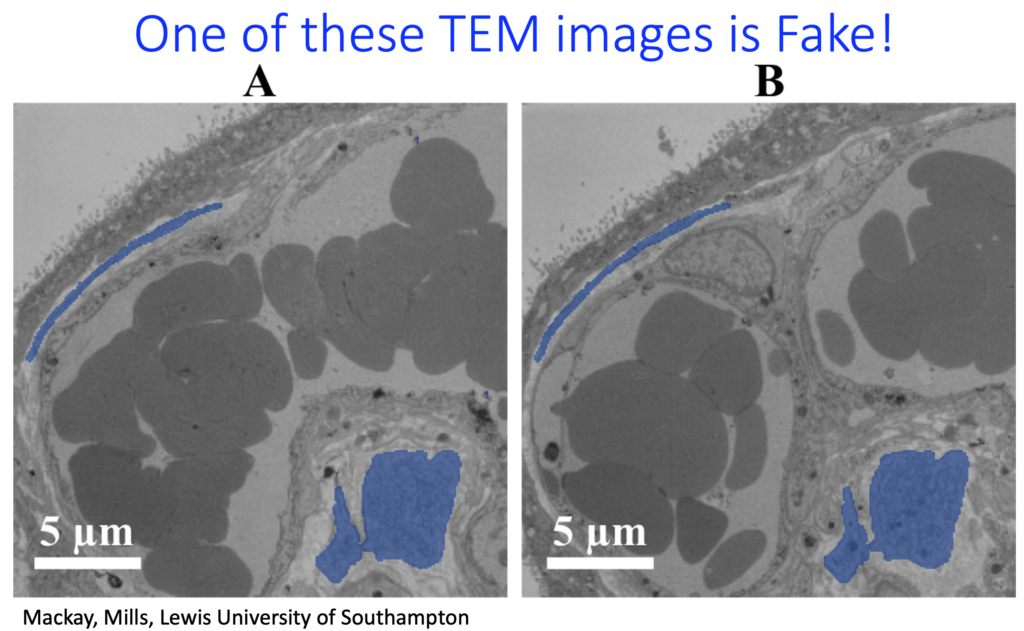
Machine-learning algorithms can effectively recognise cell types and features in placental and endometrial tissue, allowing these data to be analysed much more quickly. We trained machine-learning algorithms to make fake photorealistic electron microscope images of placental tissue. These fake images demonstrate that the trained algorithm “understands” all the spatial relationships between anatomical structures within the tissue, including intracellular components. The aim is to use the knowledge within the algorithm to explore how cells change in different physiological and pathological states.
Our research has demonstrated the potential of machine learning to speed up image analysis and provide new ways of extracting biologically exciting and clinically relevant data. In doing so, machine learning can help enhance the health of mothers and babies during pregnancy and across the life course.
Can ambulatory blood pressure measures inform shared treatment decisions in hypertension for older adults who are at risk of falls?
Dr Oliver Todd, University of Leeds

Two out of three people over 65 take treatment to lower blood pressure to prevent heart attacks and strokes. Blood pressure treatment also increases the chance of having a fall if blood pressure is lowered too much. As people get older, their blood pressure tends to rise and fall more dramatically. All this makes it hard to know how to accurately prescribe blood pressure treatment in later life.
Ambulatory blood pressure measurement (ABPM) works by equipping patients with wearable monitors that take readings two to three times an hour over the course of a day and night. Currently the output of this device is provided as a graph to the clinician but without prognostic information to aid its interpretation. We will use routinely collected ABPMs undertaken in the NHS over the past 25 years in three UK city regions. This more reflective measurement of a patient’s blood pressure will be analysed with machine-learning techniques. We will look at the 24-hour patterns of blood pressure, allowing novel pattern recognition to predict risk of heart attack and stroke, as well as falls, with potential for proactive intervention and tailoring of medicines to prevent harm.
Our research will improve the safety of blood pressure treatment in older adults at risk of falls and make it easier for patients to be involved in decisions about their treatment. The databases built will be the largest and most detailed of their kind worldwide and help us understand hypertension in older age. From this, we plan to develop future research questions that use real-world patient data, in combination with other physiological measurements, to improve patient care for older people in the UK and internationally.
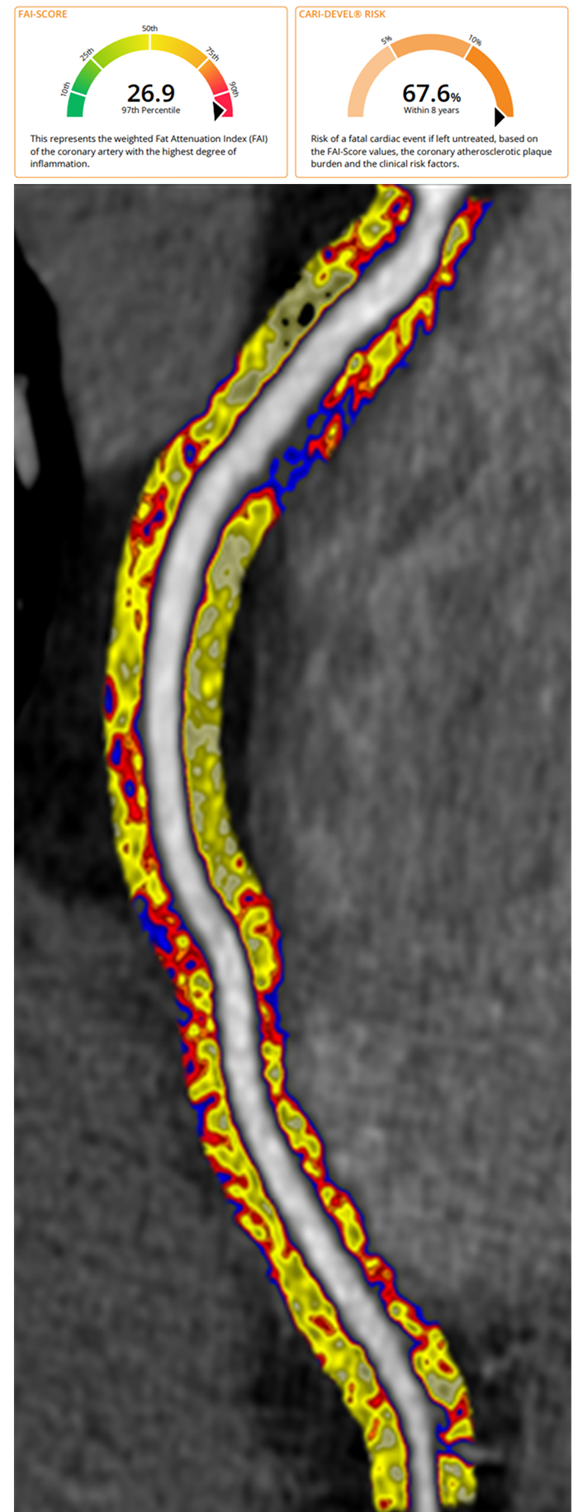
AI technology can be used to predict heart attacks from routine coronary computed tomography angiograms
Professor Charalambos Antoniades, University of Oxford
Cardiovascular disease is the number one cause of death in the UK. Heart attacks happen when inflamed atherosclerotic plaques in our heart arteries break up, blocking blood flow to the heart. Finding these inflamed plaques would allow aggressive treatment of the right patients with low-cost drugs like statins, preventing heart attacks and saving lives.
Our research team at the University of Oxford revealed that the inflamed arteries trigger changes in the texture and composition of the fat surrounding them. We then developed an artificial intelligence method that measures these changes in the fat tissue around heart arteries by analysing images obtained from coronary computed tomography angiograms (CCTAs), a test happening routinely in the NHS for the investigation of chest pain. The technology was able to predict fatal heart attacks at least eight years in advance. This would allow doctors to direct timely deployment of treatments to the right patients, preventing heart attacks and saving lives.
The technology led to the Oxford Spinout company Caristo Diagnostics, to develop a CE-marked medical device called CaRi-Heart®. This cloud-based medical device is now deployed in the first NHS Trusts, allowing doctors to predict heart attacks and focus their attention to the right patients. CaRi-Heart® currently changes medical management in about 40% of the patients undergoing the test, transforming patient care.