Aim: Patients with chronic obstructive pulmonary disease (COPD) exhibit markedly diminished exercise capacity, particularly in advanced stages, hindering their ability to perform routine activities of daily living. Previous studies have shown that skeletal muscle convective and diffusive O2 transport mechanisms play pivotal roles as peripheral determinants of exercise capacity in COPD (1, 2). This study aims to investigate whether a 12w high-intensity interval training (HIIT) intervention could reverse some of the peripheral alterations observed in patients with COPD when compared to healthy, matched controls.
Methods: Eight patients diagnosed with mild to severe COPD and eight healthy controls, untrained, matched for age, sex, and BMI, participated in this study. Baseline assessments were conducted, and the COPD patients followed by a 12-week HIIT intervention, which consisted of three weekly sessions, each comprising a 40-minute 4×4 HIIT protocol on a bicycle ergometer. Leg blood flow (Q̇leg) was assessed using Doppler ultrasound during submaximal single-leg knee-extensor exercise (KEE), with arterio-venous variables sampled across the leg. Reconstruction of the capillary oxyhaemoglobin dissociation curve was performed utilizing paired femoral arterial-venous O2 tensions and saturations for the assessment of microvascular oxygenation, including skeletal muscle O2 conductance (DsmO2) and its correction for flow (DsmO2/Q̇leg) to differentiate convective from diffusive O2 transport.
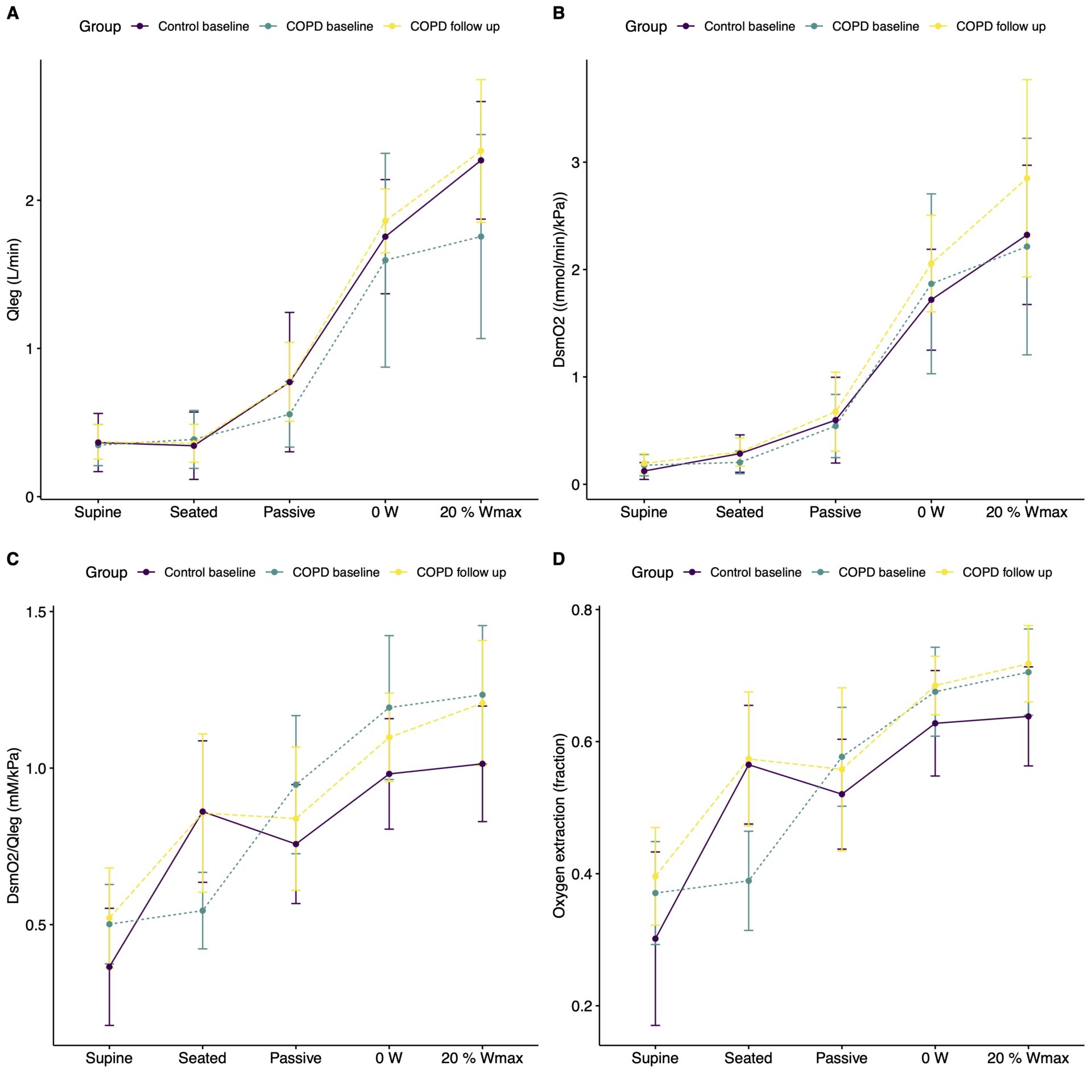
Results: The COPD and control group were similar in height, sex, and BMI, but the COPD group had more pack years (p=0.0001) as well as a lower FEV1 (p=0.002) and diffusion capacity (p=0.008). While resting values were similar, COPD patients had a higher DsmO2/Q̇leg, but a lower Q̇leg during KEE (Figure 1). After the HIIT intervention in COPD patients, the Q̇leg increase to KEE became more pronounced (428; 156 to 811 mL/min, p=0.01), but with similar O2 extraction and arterio-venous difference levels compared to pre-intervention (p=0.43). This led to a significantly higher DsmO2 to KEE compared to pre-intervention (0.65; 0.16 to1.12 (mmol/min)/kPa), p=0.01)), but with a similar change in DsmO2/Q̇leg (0.02; – 0.18 to 0.13 (mM/kPa), p=0.7) (Figure 1).
Conclusion: The diminished convective O2 transport response observed in working muscle of COPD patients can be enhanced by a 12-week HIIT intervention, so that it becomes similar to that of healthy untrained individuals without COPD. In contrast, the skeletal muscle diffusive O2 transport response in working muscle appears to be unaffected by the intervention, indicating limited skeletal muscle microvascular adaptations in COPD.