Introduction: Following the acute phase of SARS-CoV-2 infection, ,ore than a quarter of individuals suffer from persistent exercise intolerance. In a recent study, we observed that a supervised 12w high-intensity interval training (HIIT) scheme resulted in a ~4 g/m2 increase in left ventricular mass (LVM) with a corresponding improvement of functional limitations immediately after the intervention. However, there was no effect on pulmonary diffusing capacity or other lung function metrics [14]. Yet, it is unknown whether these changes persist at the long-term. We aim to investigate whether HIIT has long-term effects on cardiopulmonary function in individuals previously hospitalised for COVID-19.
Methods: We enrolled 28 patients (57 ± 11 years; 64% male) previously hospitalised for COVID-19 for this investigator-blinded randomized study with a 12-week (3 sessions/week) supervised HIIT intervention (4×4 HIIT scheme). Outcomes were assessed as the between-group change from baseline to 12mo follow-up. The primary outcome was change in LVM in grams measured by cMRI. The secondary outcomes were between-group change in pulmonary diffusing capacity for carbon monoxide corrected for haemoglobin (DL,COc), VȮ2peak, a well as the post-COVID-19 function scale (PCFS) and King’s Brief Interstitial Lung Disease (KBLID) questionnaire scores. A constrained baseline longitudinal data analysis was used to compare cardiopulmonary changes within and between groups. The study was approved by The Research Ethics Committee of the Capital Region of Denmark (H-20033733 with amendment 75068). The study conformed with the Declaration of Helsinki, and all participants provided oral and written informed consent prior to participation.
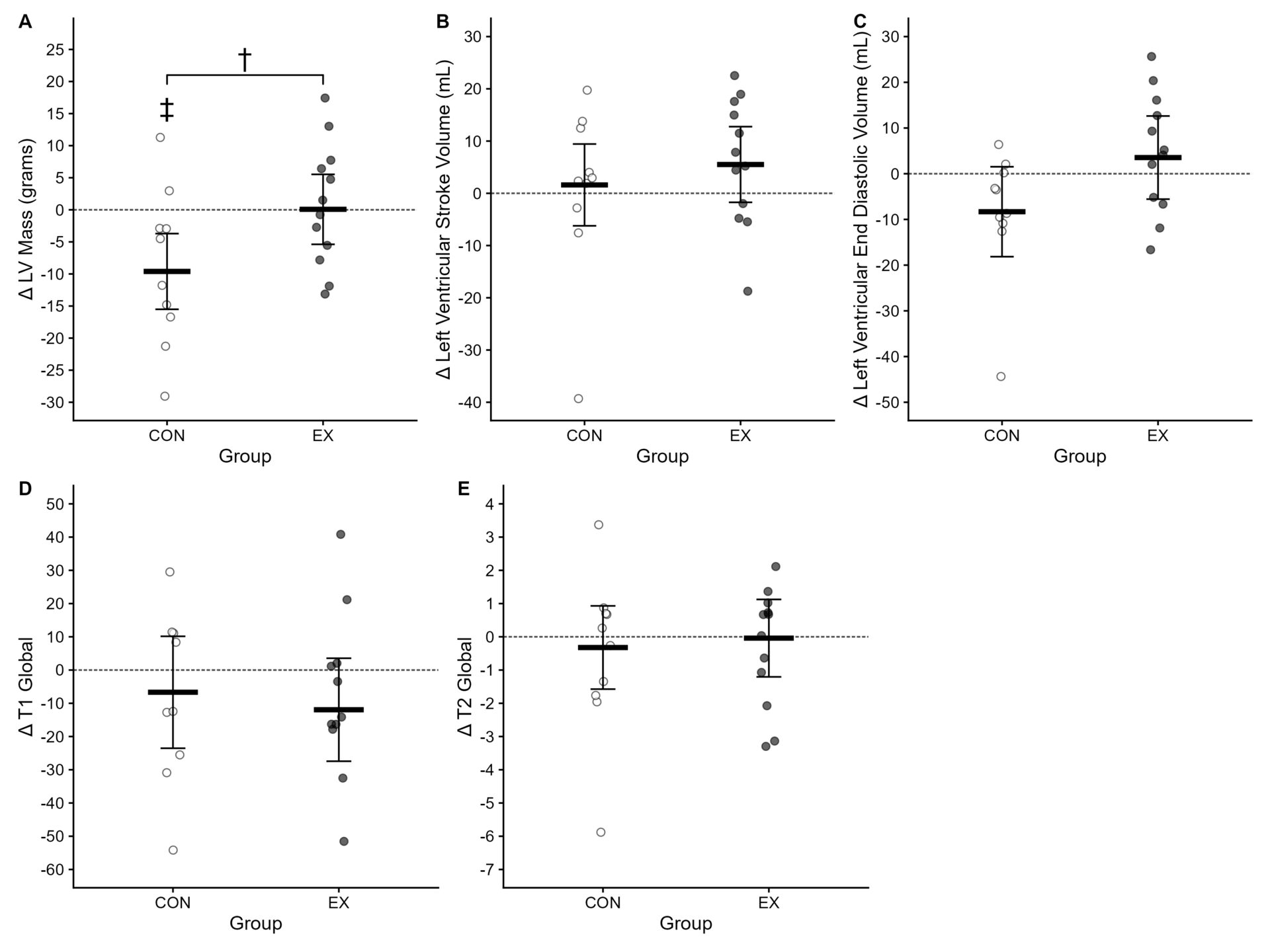
Results: Of the 28 patients invited from the main study, 23 consented to participate in the 12mo follow-up, which was completed on average 12.4±0.6mo after enrollment in the study. Ultimately, 28 participants were included in the final analysis at 12mo (HIIT: n=14, control: n=14). LVM was maintained between 3mo and 12mo follow-up in the HIIT group, whereas it decreased in the control group with a between-group difference of 9.7 [1.7; 17.6] g (p=0.018). LVEDV and LVESV showed a similar pattern, but without a significant between-group difference (Figure 1). DL,COc%pred, FEV1%pred, FVC%pred, TLC%pred and increased similarly in both groups, while RV%pred only increased in the control group.
Conclusion: In individuals previously hospitalised for COVID-19, a 12w supervised HIIT scheme leads to a persistently increased LVM reflecting physiological hypertrophy at 12mo follow-up.