Introduction: Elevated glucose levels are s major risk factor for the development of cardiometabolic disease, including type 2 diabetes. Exercise can enhance glucose uptake independently of insulin (Richter et al., 2001). Increasing physical activity, particularly through structured exercise, is widely recognized as an effective strategy to improve glycaemic control. The aim of this study was to investigate the acute and 24-hour effects of a single bout of moderate-intensity aerobic exercise (ME) and high-intensity interval training (HIIT) on glucose changes in sedentary, healthy individuals.
Methods: Following institutional ethical approval, fourteen sedentary healthy participants (4 females, age: 32.4±7.1years, BMI: 24.4±3.1kg/m2, VO2max: 39.5±5.6ml/min/kg) wore continuous glucose monitors (CGM, Abbot FreeStyle Libre) and wearable fitness trackers (Fitbit Charge 4) to estimate interstitial glucose levels and track total sleep time, respectively, for 14 consecutive days. Mean amplitude of glycaemic excursions (MAGE), standard deviation (SD) and coefficient of variation (CV) from CGM recordings were calculated to assess the 24-hour glucose variability (GV). Each participant performed, in the morning, either 30min of ME or a HIIT session, each followed by 60 minutes of rest. Each session was separated from the other by at least 3 days, and the order of the sessions was randomised. The ME was performed at 60%VO2max with continuous cycling on a cycle ergometer, while HIIT was at performed 60%VO2max with 4-6s of maximal effort performed every 2min. Capillary blood glucose (BG) was measured 15min before and every 10min during the exercise and recovery periods.
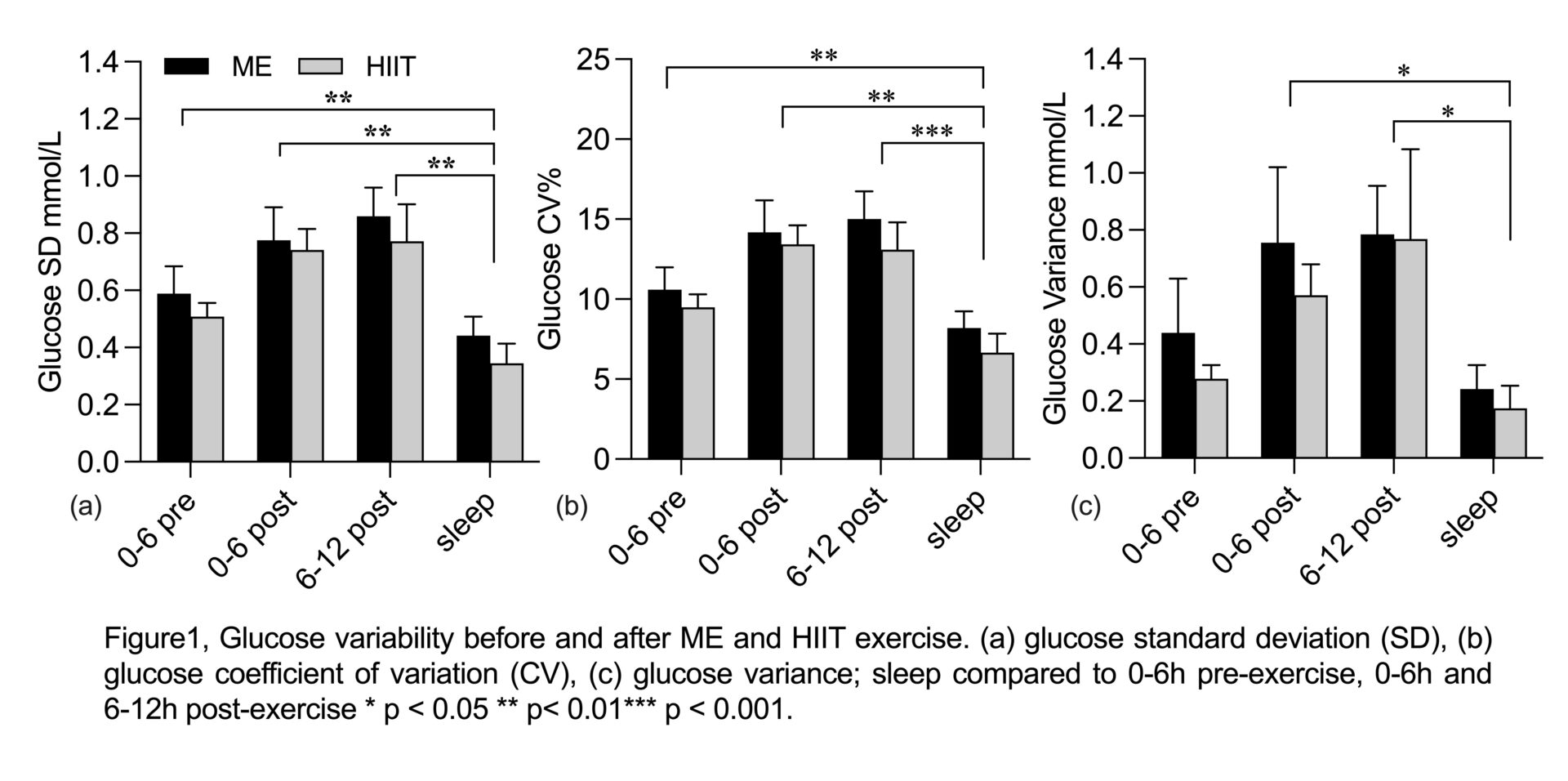
Results: HIIT resulted in a higher rate of perceived exertion than ME (15.2±1.9 vs 12.6±1.7, p<0.001). During the acute recovery period, an increase in BG was observed at 30 (5.1mmol/L), 40 (5.0mmol/L) and 60min (5.1mmol/L) post-exercise when compared to the 0min post-exercise (4.6 mmol/L) following ME (all p<0.05), but no changes were observed in HIIT. Regarding the 24h and sleep GV, both exercise days were similar to the control day and no GV differences were observed between the 0-6h and 6-12h post-exercise following both exercise modalities. However, a decline in GV was observed during sleep compared to the 0-6h pre-exercise (CV & Variance), 0-6h and 6-12h post-exercise (SD, CV & Variance; all p<0.05) (figure 1).
Discussion: The acute effect of ME resulted in a slower recovery of BG compared to HIIT, particularly within the short-term recovery period (up to 30min post-exercise). However, no significant effect of ME or HIIT on 24h GV when compared to the control day was observed, nor on 0-6h & 6-12h post-exercise GV when compared to the 0-6h pre-exercise period. A reduction in GV during sleep was also observed following both exercise modalities. These findings suggest that while ME and HIIT may affect acute glucose recovery differently, their effects on 24h glycaemic control remain comparable. This suggests the potential for tailored exercise regimens to improve immediate glucose metabolism without altering daily GV.