Introduction: Non-alcoholic fatty liver disease (NAFLD), a spectrum of liver disorders ranging from simple steatosis to steatohepatitis related cirrhosis is emerging as the leading cause of liver morbidity and mortality. While the exact cause of the disorder is presently unknown, obesity and other components of the metabolic syndrome are suggested to play causal role in its incidence and progression. Presently, there is no medication for NAFLD and this has prompted research efforts to understand its pathogenesis and find cure for the disorder. Acriflavine, has been reported to possess activity in the treatment of obesity, right ventriclar hypertrophy and right ventricle systolic pressure. Based on this, we hypothesized that acriflavine would be an effective remedy for NAFLD.
Aim/objectives: This study was designed to explore the pathogenesis of NAFLD, the potentials of acriflavine to act as remedy for the disorder, and to investigate probable mechanisms through which this might occur in wistar rats.
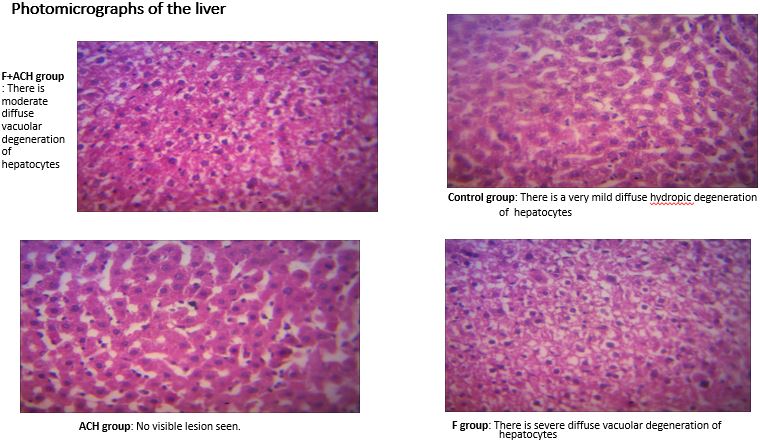
Methods: Twenty male Wistar rats (100-120g) were randomly divided into four groups (n=5/group) namely: Control group given feed and water, Fructose (F) group given high carbohydrate high fat diet (HCHFD) and fructose sweetened drink (FSD) (0.10g/mL), Acriflavine (ACH) group given feed, water and acriflavine (100 mg/kg/day), and F+ACH group given HCHFD, FSD and acriflavine (100mg/kg/day) for 14 weeks. At 14 weeks, blood pressure, heart rate, anthropometric variables and fasting blood glucose were determined. Diazepam (0.4 mg/kg) and ketamine (40 mg/kg) administered intramuscularly into the left hind leg were used as anaesthesia. Serum lipids, proteins, insulin, bilirubin, and liver enzymes, HOMA-IR, liver weight, lipids, inflammation and oxidative stress were determined. Liver histopatholological examination was also done. The procedures of the experiment were endorsed by University of Ibadan Animal Care and Use Research Ethics Committee (UI-ACUREC/19/0140). Data were compared with ANOVA and P0.05 was considered statistically significant. The procedures of the experiment also conform to the National Institutes of Health (NIH) Guide for the Care and Use of Laboratory Animals.
Results: systolic (p<0.0001), diastolic (p=0.0003), and mean blood pressures (p<0.0001), heart rate (p=0.0004), body weight gain (p=0.002), abdominal circumference (p=0.0007), total abdominal fat (p=0.004), blood glucose (p<0.0001), serum insulin (p=0.0002), triglyceride (p=0.0011), total cholesterol (p=0.024), bilirubin (p=0.0457), aspartate aminotransferase (p=0.0165), alanine aminotransferase (p=0.0471), alkaline phosphatase (p=0.0063), total protein (p=0.0388), globulin (p=0.0058), HOMA-IR (p<0.0001), liver weight (p=0.025), TNF-α (p=0.0086) and IL-6 (p=0.0074), hepatic lipids and oxidative stress markers increased significantly in F group when compared with Control while most of them reduced in ACH treated rats when compared with F rats.
Conclusion: The findings of this study showed that a “multiple hit” mechanism underlie NAFLD and also that acriflavine improved NAFLD modestly. This beneficial effect was largely due to the prevention of obesity and components of the metabolic syndrome.