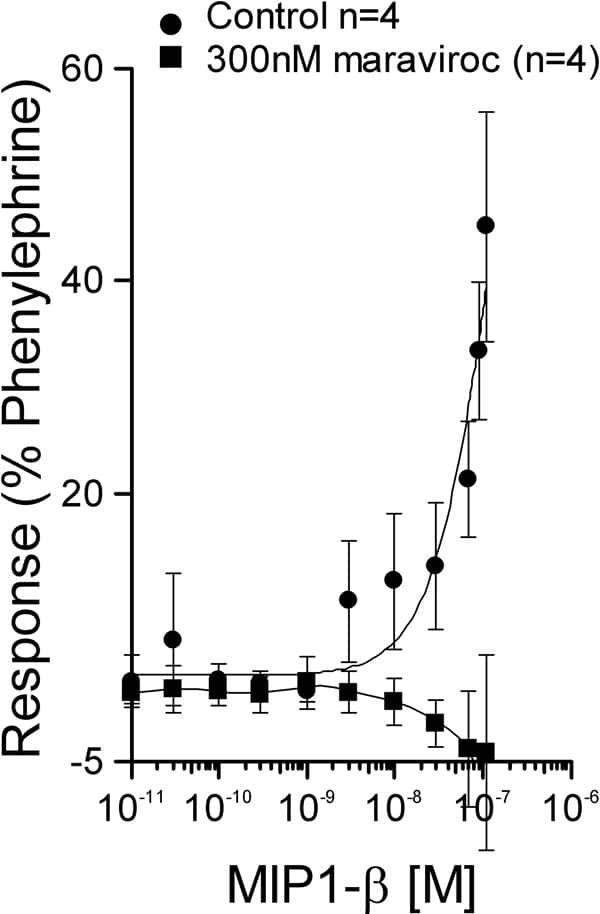
HIV-infected individuals are at increased risk of cardiovascular events, possibly owing to accelerated atherosclerosis. The mechanisms involved are unclear. The chemokine receptor CCR5 is a major co-receptor for the HIV virus. Interestingly, CCR5 deficiency results in a reduction in diet-induced atherosclerosis in mice (Braunersreuther et al., 2007) and CCR5 and its ligand MIP1-β are expressed in human vascular smooth muscle (Schecter et al., 2000). A direct effect on vascular tone of chemokines has not been reported. Human saphenous vein (SV) is a widely used graft in patients with coronary artery disease however, grafts, particularly SV, exhibit a form of accelerated atherosclerosis making this blood vessel a useful model of disease. In initial experiments we have determined whether MIP1-β has direct constrictor/dilator action in SV and confirmed that this is a CCR5 mediated action using the selective antagonist maraviroc (UK-427,857; Dorr et al., 2005). Rings (4mm) of human SV were denuded of their endothelium and mounted in organ baths, containing Krebs’ solution at 37°C, for isometric tension recording. Following a normalisation procedure to optimise basal tension, endothelium removal was confirmed by the absence of a vasodilator response to ACh in phenylephrine constricted veins. Cumulative concentration-response curves (CRC) were then constructed to MIP1-β (10-11-1.1×10-7M). In adjacent rings of SV from some patients, 300nM maraviroc or vehicle (DMSO 0.01%) were added to the bathing medium and cumulative CRC to MIP1-β constructed 30 minutes later. In additional experiments, CRC to MIP1-β were constructed in SV that had been preconstricted with endothelin-1 (10nM) and experiments terminated by addition of 30μM SNAP. Vasoconstrictor responses were expressed as a %phenylephrine and vasodilator responses as %reversal of ET-1 constriction. Data were analysed using FigSys (Biosoft, Cambridge, UK) to determine values of pD2 and maximum response. n-Values are the number of patients from whom tissue was obtained. In ET-1 constricted SV, MIP1-β did not elicit direct vascular smooth muscle relaxation over the concentration range tested. In contrast MIP1-β produced a concentration-dependent contraction of SV with pD2 of 7.73±0.17 (n=12). In the presence of 300nM maraviroc (n=4), the constrictor response to MIP1-β was abolished (Fig 1). These data reveal a previously unidentified role for the chemokine MIP1-β as a potent constrictor of human SV, an effect mediated through the CCR5 receptor present on vascular smooth muscle.
Life Sciences 2007 (2007) Proc Life Sciences, C98
Research Symposium: Novel function of the inflammatory chemokine MIP1-β, a ligand for the HIV co-receptor CCR5, as a vasoconstrictor of human blood vessels: antagonism by maraviroc
J. Maguire1, R. E. Kuc1, S. D. Katugampola2, K. L. Jones1, R. W. Mansfield2, C. M. Napier2, A. P. Davenport1
1. Clinical Pharmacology Unit, University of Cambridge, Cambridge, United Kingdom. 2. Pfizer Global Research and Development, Sandwich, Kent, United Kingdom.
View other abstracts by:
Fig. 1 Antagonism of MIP1-β by maraviroc in SV
Where applicable, experiments conform with Society ethical requirements.