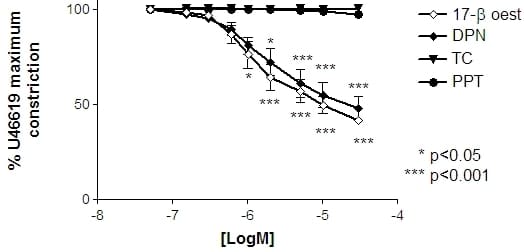
An acute vasodilatory action of 17-β oestradiol in many vascular beds depends upon oestrogen receptor (ERα and ERβ) activation. The role of 17-β-oestradiol in regulating human vascular tone is of interest in many physiological settings including the uteroplacental unit. Maternal serum levels of 17-β oestradiol, and uterine blood flow, increase during pregnancy and 17-β oestradiol acutely relaxes uterine arteries in vitro. Alternatively, little is known of 17-β oestradiol influences on placental vascular tone. As the placenta lacks autonomic regulation, arterial tone is controlled by locally derived substances one of which may be oestrogen. The placenta also offers a source of non-pathophysiological blood vessel specimens, and it was therefore pertinent to investigate if 17-β oestradiol and agonists of ERα or ERβ, have a role in the regulation of placental arterial tone. Chorionic plate arteries (200-500µm) were dissected from placentas collected (n=12, with LREC approval) from normal term pregnancies. Vessels were bathed in Physiological Salt Solution (PSS, 5%CO2/95%air, 37oC) and isometrically constricted with the thromboxane receptor ligand U46619 (1µM). Upon stable constriction, incremental doses (0.05-30μM) of 17-β oestradiol, 17-α oestradiol (a putatively inactive stereo-isomer), ERα agonist propylpyrazoletriyl (PPT) or ERβ agonist diarylpropionitrile (DPN) were applied. Vessels were washed with PSS, re-constricted with U46619 and exposed to a single dose (30µM) of 17-β oestradiol, 17-α oestradiol, PPT or DPN. In a subset of experiments, the influence of 17-β oestradiol, 17-α oestradiol, PPT or DPN on U46619-induced Ca2+-sensitisation (pCa 6.7) of α-toxin permeabilised arteries was studied. Pre-constricted arteries (n=6) significantly relaxed in response 17-β oestradiol from 1µM-30µM (p<0.001, 2 way anova of Arcsine transformed data, bonferroni post hoc test) and to DPN from 2µM-30µM (Figure 1). Similar relaxations to PPT or 17-α oestradiol were not evident. Separate single dose 30µM exposure to 17-β oestradiol (n=6) or DPN also relaxed pre-constricted arteries, to 41.8±1.1% or 50.5±3.9% respectively (P<0.01, one way anova) of U46619 max-constriction. In permeabilised arteries (n=5), none of the agents significantly relaxed U46619-induced tone at pCa 6.7. In summary, the acute relaxation of human placental vascular tone by 17-β oestradiol may, in part, be due to signalling via ER-β but does not appear to involve direct activation on smooth muscle of Ca2+-desensitisating pathways. It remains to be seen if similar actions are evident in other human arterial vascular beds but nonetheless places oestradiol as a potential endocrine regulator of human placental vascular tone.
University of Cambridge (2008) Proc Physiol Soc 11, PC144
Poster Communications: 17β oestradiol-dependent acute relaxations of human arteries in vitro: a role for ERβ?
J. J. Corcoran1, M. Westwood1, S. C. Robson2, M. Sweeney2, M. J. Taggart2
1. Maternal and Fetal Health Research Centre, University of Manchester, Manchester, United Kingdom. 2. Institute of Cellular Medicine, Newcastle University, Newcastle, United Kingdom.
View other abstracts by:
Figure 1: Dose-response curves to 17-β oestradiol PPT and DPN with matched time controls. Significant relaxation (*) was achieved when exposed to 17-β oestradiol or DPN.
Where applicable, experiments conform with Society ethical requirements.