Physiology News Magazine
Vascular adaptations and exercise training: how to convince your cardiologist that physiology is important
Features
Vascular adaptations and exercise training: how to convince your cardiologist that physiology is important
Features
Danny Green, Mark Black, & Tim Cable
Liverpool John Moores University
https://doi.org/10.36866/pn.74.27
A physiologist who works with cardiologists sometimes needs a thick skin. I vividly recall the first talk I gave, as an enthusiastic PhD student, to a room full of busy interventional cardiologists. After 30 minutes proselytizing the ‘undoubted benefits of exercise and cardiac rehabilitation’, the Professor of Cardiology stood up and solemnly stated ‘Everyone knows that one is born with a certain number of heart beats, and the more you exercise the quicker they get used up’. I was left to consider whether the Professor, my PhD supervisor, was entirely committed to our planned exercise training studies!
During the more recent era of cardiovascular (CV) ‘block-buster’ drugs, any suggestion that exercise may be important in primary or secondary prevention of cardiovas-cular disease was likely to be met with the assertion that ‘Cardiac rehabilitation should consist of making sure patients are compliant with their drug regimes’. To a GP or a Specialist who has been educated, overtly or otherwise, through an era of emphasis on drugs for CV risk factor modification, it is logical that an intervention such as exercise, which has relatively modest impacts on such risk factors, should have to justify itself. Of course this view is based on the notion that the effects of exercise training (or physical activity) are secondary in nature: that is, exercise exerts its benefits by modifying well-established risk factors like blood pressure or lipid levels.
It is true that the effects of exercise on traditional risk factors are, on average, relatively modest compared to the direct impact of drug treat-ments (Thompson et al. 2003; Green et al. 2008a). Even if exercise is a ‘poly-pill’ and the benefits on each risk factor summate, they probably do not approach the combined impact of drug treatment with agents like statins and angiotensin converting enzyme inhibitors. Nonetheless, primary and secondary prevention analyses suggest that exercise (or cardio-pulmonary fitness) is associated with around 30% CV risk reduction, relative to inactivity or ‘usual (!)’ care (Green et al. 2008a). In secondary prevention (cardiac rehabilitation) studies, this benefit is additional to that associated with optimal contem-porary medical and interventional management (Taylor et al. 2004). Clearly exercise decreases CV risk. But how?
One lead was provided by a recent analysis (Mora et al. 2007) which reported that changes in established and novel risk factors explained only about 50% of the cardiovascular risk reduction associated with exercise. That is, around half of the risk reduction associated with exercise is unaccounted for and cannot be explained by ‘secondary’ impacts of exercise on establish risk factors (Fig. 1).
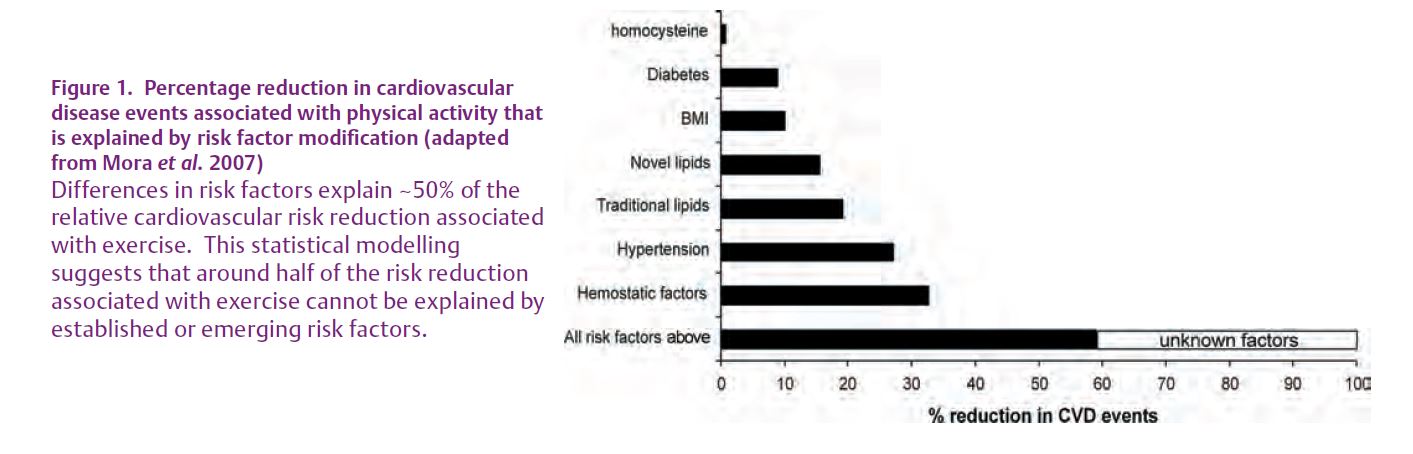
Perhaps it’s time to consider direct impacts of exercise on the vasculature?
Exercise is associated with changes in both vascular function and structure. For example, it is well established that training programs enhance endothelial function (Hambrecht et al. 2003), although the type of exercise or the patient groups involved may influence the magnitude or indeed presence of any benefit. Generally, beneficial effects of exercise training have been observed in resistance and conduit arteries of both skeletal and coronary vascular beds in patients with risk factors or CV diseases, in whom vascular function may be impaired a priori. Benefits in younger or healthier subjects have been less universally observed. Changes in arterial size, or arterial remodelling, also occur with exercise training and may also be endothelium dependent (Green et al. 2004).
Hence, although there is strong evidence in humans that exercise training has direct effects on vascular function and size, some inconsist-encies exist in the literature and many questions remain. What is the stimulus responsible for training effects on the vasculature? Do the functional and structural changes interact or co-exist? Are adaptations equally apparent at all levels of the arterial tree?

What is the stimulus responsible for training effects on the vascu-lature? Repetitive exposure to increased shear stress may be a key physiological stimulus to vascular adaptation in humans. Acute exercise is associated with increased blood flow and driving pressure, but the blood flow (and shear) profile associated with exercise may depend upon the nature of the exercise itself and whether the vascular bed feeds active or inactive muscle (Fig. 2). Leg exercise, for example, induces changes in upper limb blood flow which include a substantial retrograde flow component (Green et al. 2005). In contrast, hand-grip exercise is associated with increased anterograde flows and shear, but modest change in retrograde flows. This difference in flow patterns may explain the observation that many exercise training studies involving localised handgrip training have not produced significant improvement in endothelial function, whilst studies which have utilised large muscle group exercise involving the lower limbs (cycling, running, etc), have often observed improvements in vasodilator function and/or capacity, even in the untrained upper limbs (Green et al. 2008b).

Do functional and structural changes interact or co-exist? Toni Tinken and Dick Thijssen recently investigated another explanation for the inconsistencies in exercise training findings in humans, related to the time-course of change in function and structure (Tinken et al. 2008). In young men, conduit artery function improved during the early stages of exercise training, but then normalised as arterial outward remodelling occurred (Fig. 3). As originally suggested by Harold Laughlin and colleagues, it seems likely that early functional adaptations may be superseded by arterial remodelling, which enables function to normalise at the larger structural set-point. The lack of difference in function when assayed at later time points may also explain the disparity between studies in the literature regarding the impact of training, particularly in healthy younger subjects.
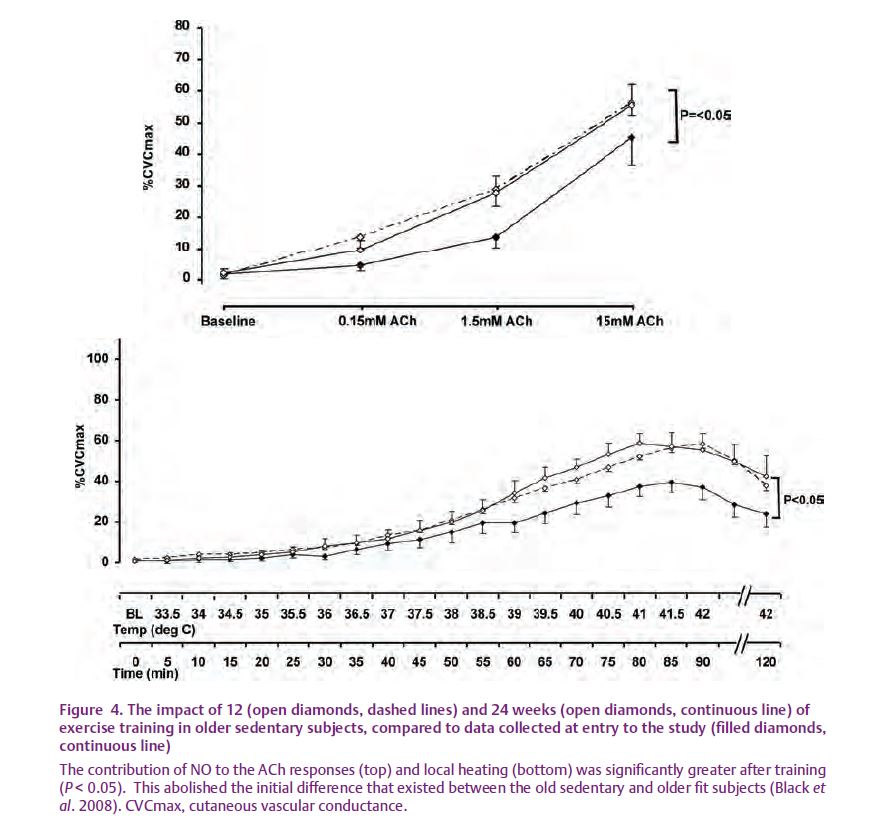
Are adaptations equally apparent at all levels of the arterial tree? In resistance arteries, improvements in vascular function and arterial remodelling may contribute to the hypotensive effect of training, apparent at rest, and also the increase in vascular conductance which absorbs large training-induced increases in cardiac output manifest during exercise. In conduit arteries, direct effects of exercise training on endothelial function may decrease macrovascular risk. A separate question relates to the possible impact of exercise training on microvascular function. Mark Black recently addressed this question in his PhD work by comparing healthy young subjects to exercise-trained and fit older subjects and also older sedentary controls (Black et al. 2008). The latter group were subsequently randomised to an exercise training or control group for a period of 24 weeks. The impact of localised heating and also acetylcholine infusion on skin vasodilator function was assessed. NO blockade was performed to characterise the contribution of this substance to microvascular changes observed. Sedentary ageing was associated with diminished NO-mediated vasodilator function in response to both heating and ACh admin-istration, whilst exercise training in the older sedentary subjects reversed this (Fig. 4). Maintaining fitness as you age, or taking up exercise training, improves micro-vascular function. These findings provide a mechanistic rationale for the promotion of exercise for the prevention of microvascular disease in humans and may be important if the large increases in obesity and type 2 diabetes eventuate in the coming decades, as predicted.
Final word: If we are to optimise the design of interventions aimed at preventing cardiovascular disease/s, then it is important to understand the physiology which underpins vascular adaptations. Exercise is important, even for cardiologists. A study from Rainer Hambrecht’s group (Hambrecht et al. 2004) compared the effects of optimal interventional management of coronary artery disease, including stenting, to exercise training alone. Both groups received comparable medical management. After 12 months, the ‘stent’ group exhibited markedly decreased stenosis diameter (81% to 2%), whereas the exercise training group, who did not have an angioplasty or a stent, exhibited no change in lesion size (78% to 77%). Nonetheless, significantly higher event-free survival occurred with exercise training (88% vs 70%). It seems that exercise exerts beneficial effects on vascular function/remodelling and disease progression in the entire arterial bed, whereas stents apply a band-aid. The authors, a group of cardiologists, concluded that in contrast to exercise training, coronary interventions must be regarded as a palliative therapy with regard to the underlying process of atherosclerosis.
References
Black MA, Green DJ & Cable NT (2008). Exercise prevents age-related decline in nitric oxide-mediated vasodilator function in cutaneous microvessels. J Physiol 586, 3511–3524.
Green DJ, Bilsborough W, Naylor LH, Reed C, Wright J, O’Driscoll G & Walsh JH (2005). Comparison of forearm blood flow responses to incremental handgrip and cycle ergometer exercise: Relative contribution of nitric oxide. J Physiol 562, 617–628.
Green DJ, Cable NT, Joyner MJ & O’Driscoll G (2008a). Exercise and cardiovascular risk re-duction: Updating the rationale for exercise. J Appl Physiol 105, 766–768.
Green DJ, Maiorana AJ & Cable NT (2008b). Exercise training does induce vascular adap-tations beyond the active muscle beds. J Appl Physiol 105, 1002–1004.
Green DJ, Maiorana AJ, O’Driscoll G & Taylor R (2004). Effects of exercise training on vascular endothelial nitric oxide function in humans (Topical Review). J Physiol 561, 1–25.
Hambrecht R, Adams V, Erbs S, Linke A, Kran-kel N, Shu Y, Baither Y, Geilen S, Thiele H, Gum-mert JF, Mohr FW & Schuler G (2003). Regular physical activity improves endothelial function in patients with coronary artery disease by in-creasing phosphorylation of endothelial nitric oxide synthase. Circulation 107, 3152–3158.
Hambrecht R, Walther C, Möbius-Winkler S, Gielen S, Linke A, Conradi K, Erbs S, Kluge R, Kendziorra K, Sabri O, Sick P & Schuler G (2004). Percutaneous coronary angioplasty compared with exercise training in patients with stable coronary artery disease: A random-ized trial. Circulation 109, 1371–1378.
Mora S, Cook N, Buring JE, Ridker PM & Lee IM (2007). Physical activity and reduced risk of cardiovascular events: Potential mediating mechanisms. Circulation 116, 2110–2118.
Taylor RS, Brown A, Ebrahim S, Jolliffe J, Noorani H, Rees K, Skidmore B, Stone JA, Thompson DR & Oldridge N (2004). Exercise-based rehabilitation for patients with coronary disease: sys-tematic review and meta-analysis of random-ized controlled trials. Am J Med 116, 682–692.
Thompson PD, Buchner D, Pina IL, Balady GJ, Williams MA, Marcus BH, Berra K, Blair SN, Costa F, Franklin B, Fletcher GF, Gordon NF, Pate RR, Rodriguez BL, Yancey AK & Wenger NK (2003). Exercise and physical activity in the prevention and treatment of atherosclerotic cardiovascular disease. A statement from the Council on Clinical Cardiology (Subcommittee on Exercise, Rehabilitation, and Prevention) and the Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity). Circulation 107, 3109–3116.
Tinken TM, Thijssen DHJ, Black MA, Cable NT & Green DJ (2008). Conduit artery functional adaptation is reversible and precedes structural changes to exercise training in humans. J Physiol 586, 5003–5012.