
Physiology News Magazine
Inspiratory muscle training as an ergogenic aid: credible at last?
Recent evidence points to an important role for respiratory muscle work in limiting exercise tolerance. Alison McConnell (below) proposes that it is time to start thinking differently about the role of inspiratory muscle training in alleviating this limitation
Features
Inspiratory muscle training as an ergogenic aid: credible at last?
Recent evidence points to an important role for respiratory muscle work in limiting exercise tolerance. Alison McConnell (below) proposes that it is time to start thinking differently about the role of inspiratory muscle training in alleviating this limitation
Features
Alison K McConnell
Centre for Sports Medicine & Human Performance, Brunel University, Uxbridge, UK
https://doi.org/10.36866/pn.68.26

For most of the 20th century, exercise physiologists viewed the respiratory system as one that was the exception to the rule of symorphosis (structural design is matched to functional demand). After all, at sea level, oxygen transport is not limited by the diffusion of oxygen, and human beings appear to have considerable breathing reserve, even at maximal exercise. What, then, might be the point of training the respiratory pump muscles? The past decade has witnessed a considerable advancement in our understanding of the limitations imposed by respiratory muscle work, as well as providing insights into the mechanisms by which specific training of the respiratory pump elicits improvements in exercise tolerance.
Research on respiratory muscle training (RMT) has its origins in the 1970s, when early studies sought to demonstrate that the respiratory muscles were responsive to specific training. Later research sought to evaluate the potential benefits of such training with respect to exercise tolerance in both healthy people and patients with respiratory disease. Up until the late 1990s, the literature on RMT in healthy young adults was contradictory to say the least(McConnell & Romer, 2004b). Poor research design and inappropriate outcome measures had created a very ‘mixed bag’ of data that only served to confirm the perceived wisdom that breathing does not limit exercise tolerance. The picture was equally murky with respect to research on patients with lung disease, but interpretation of this body of research was also hampered by a lack of rigorously conducted studies (see McConnell & Romer, 2004a). A turning point in research on RMT came during the late 1990s, when more reliable methods of training became more widely used (specifically pressure threshold training) and a more rigorous approach to research design was adopted.
My own group has had a particular interest in the potential application of RMT as an ergogenic aid, i.e. as a performance-enhancing intervention in athletes. An important aspect of research on the ergogenic properties of interventions is to establish outcome measures that are not only reliable, but also have the external validity to make them relevant to athletic performance. In this context, time trials (performance against the clock) provide both validity and, in the right hands, reliability. The disadvantage of time trials is that the effect size of a performance change is generally very small (<5%), which means that participants must have excellent pacing skills and be accustomed to reproducing truly maximal time trial performances.
The first study to examine the influence of RMT on time trial performance used rowing as the exercise modality, and chose well-trained oarswomen as participants (Volianitis et al. 2001). The advantage of using well-trained athletes is that the reliability of their time trials is very high. A single-blind placebo-controlled design was implemented, and performance was assessed using two rowing ergometer time trials in the laboratory. The 11 week period of pressure threshold inspiratory muscle training (IMT) increased the distance covered during a 6 minute all-out effort by 1.9% above placebo, and the time taken to cover 5,000 m improved by 2.2%. In addition, there were accompanying reductions in blood lactate concentration and breathing effort during a separate ergometer trial incorporating a series of fixed work rates. Finally, IMT also reduced inspiratory muscle fatigue induced by the 6 minute time trial (from an ~11% deficit in strength to ~3%), despite the fact that the athletes had completed the time trial more quickly.
In a subsequent study on well-trained male cyclists, the rigour of the research design was improved by using a double-blind placebo-controlled design, and by quantifying both the IMT and the whole-body training (Romer et al. 2002). The latter was to ensure that any changes in exercise performance could not be ascribed to changes in the athletes’ whole-body training. The performance outcome measures in this study were a 20 km and a 40 km cycling time trial, which were simulated under laboratory conditions. After the 6 week period of IMT, the 20 km and 40 km time trial performances improved by 3.8% and 4.6% above placebo, respectively. The study also demonstrated attenuation of both respiratory and whole-body effort sensations, and a reduction in exercise-induced inspiratory muscle fatigue. Thus, in both oarswomen and male cyclists, IMT induced a range of physiological and perceptual changes that were consistent and repeatable.
Neither the rowing nor the cycling study demonstrated any change in maximal oxygen uptake (VO2max) after IMT, which is consistent with observations of other investigators (see McConnell & Romer, 2004b). Some exercise physiologists interpreted this finding as a weakness of the studies; after all, how could training the respiratory pump increase exercise performance without increasing maximal oxygen uptake? Of course, a change in VO2max would have completely contradicted our understanding of the factors that limit oxygen transport, since the participants were not diffusion limited. For a time it was thought that the answer may lie in a change in the lactate threshold, which is the other key mechanism by which exercise performance improvements are normally achieved following whole-body training. However, in a carefully conducted study we later showed that inspiratory muscle training did not improve the lactate threshold (McConnell & Sharpe, 2005).
These observations led to the conclusion that the mechanism underlying the apparent ergogenic effect of IMT must lie outside our conventional view of training-induced improvements in performance, i.e. it was not due to improvements in VO2max and/or the lactate threshold. During this same period of the 1990s, Jerry Dempsey’s group at the University of Wisconsin was undertaking some outstanding and elegant research into the influence of respiratory muscle work upon exercise tolerance. A review of this research was published in Physiology News (65, 25–27) and will not be rehearsed again here – suffice to say Jerry Dempsey and his colleagues have now provided very convincing evidence for the existence of an inspiratory muscle metaboreflex that can result in a blood flow ‘steal’ from the locomotor muscles. Could inspiratory muscle training be exerting its ergogenic effect by delaying or attenuating this reflex?
Hitherto, studies of the inspiratory muscle metaboreflex had been confined to models that studied vascular responses to the metaboreflex in either the resting limb, or during whole body cycling at maximal exercise. Thus, there was evidence that fatiguing inspiratory muscle work was capable of inducing vasoconstriction in the resting limb, and under conditions where cardiac output was maximal. However, it was unclear whether the metaboreflex could override the functional hyperaemia of exercise under conditions where there was cardiac output reserve. Furthermore, even if the metaboreflex did operate under such conditions, it was far from clear whether IMT could modulate its operation.
In our most recent study we have examined these questions using an isolated human lower leg model (McConnell & Lomax, 2006). Our basic premise was that if the inspiratory muscle metaboreflex induced a functionally meaningful reduction in limb vascular conductance, then the resulting impairment of limb blood flow should accelerate limb fatigue.
Furthermore, if IMT modulated the reflex, then the fatigue profile of the limb should also be modulated after IMT. To validate our limb fatigue model (plantar flexion), we first assessed its sensitivity to mechanical restriction of blood flow. In addition, we confirmed the ability of a fatiguing inspiratory muscle-loading protocol (IMF) to activate the inspiratory muscle metaboreflex. Following this, a number of manipulations of the pre-plantar flexion conditions were implemented: (1) a bout of IMF immediately prior to the plantar flexion, and (2) an identical bout of IMF followed by a 30-minute period of rest (to allow the metaboreflex to dissipate) before plantar flexion. After a 4 week period of IMT, condition (1) was repeated. In addition, we implemented a final condition in which the intensity of the inspiratory muscle loading was increased to account for the training-induced improvement in inspiratory muscle strength.
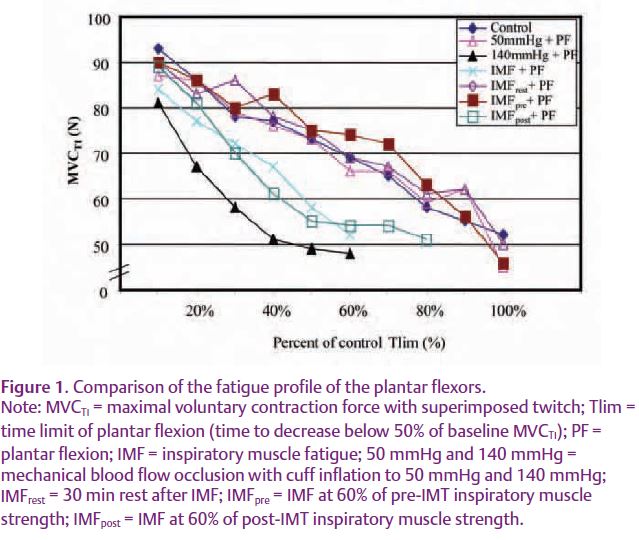
When plantar flexion was preceded immediately by IMF, the rate of plantar flexor fatigue was accelerated (Fig. 1). When a 30 minute period of rest was given between the IMF and plantar flexion, the fatigue profile was not significantly different to control. Similarly, after IMT, the same bout of IMF failed to induce any change in the rate of plantar flexion fatigue. In contrast, when the intensity of the IMF was increased to take account of the training-induced improvement in strength, the rate of plantar flexion fatigue was once again accelerated. These data support the notion that the inspiratory muscle metaboreflex operates at exercise intensities where there is cardiac output reserve. Furthermore, they suggest that IMT changes the threshold of inspiratory muscle work required to elicit the vasomotor response to activation of this metaboreflex. Thus, the most important determinant of the functional repercussions of inspiratory muscle work appears to be the relative intensity of that inspiratory muscle work.
In summary, RMT research has been hampered by the results of some poor studies that have generated contradictory data. In addition, there has been a natural scepticism about an intervention that appeared to fly in the face of exercise physiologists’ understanding of the role of the respiratory pump in oxygen transport. However, respiratory muscle work has far wider repercussions than were previously appreciated, and it is now known that these muscles contribute to both the metabolic demand and sensory experience of exercise. Recent studies suggest that IMT generates improvements in exercise tolerance through two main mechanisms, which are probably also interlinked: (1) attenuation of effort sensations (exercise feels easier after IMT) and (2) attenuation of the inspiratory muscle metaboreflex leading to a preservation of limb blood flow during exercise.
The role of RMT in enhancing exercise performance in athletes, as well as exercise tolerance in patients with dyspnoea, increased work of breathing, and/or circulatory limitations (e.g. chronic obstructive pulmonary disease, chronic heart failure) has been made considerably more credible by newly acquired insights into the wider consequences of exercise-induced inspiratory muscle work.
Acknowledgements
The author acknowledges a beneficial interest in the POWERbreathe® inspiratory muscle trainer in the form of a royalty share on license income to the University of Birmingham. She also provides consultancy services to Gaiam Ltd.
References
McConnell AK & Lomax M (2006). The influence of inspiratory muscle work history and specific inspiratory muscle training upon human limb muscle fatigue. J Physiol 577, 445–457.
McConnell AK & Romer LM (2004a). Dyspnoea in health and obstructive pulmonary disease: the role of respiratory muscle function and training. Sports Med 34, 117–132.
McConnell AK & Romer LM (2004b). Respiratory muscle training in healthy humans: resolving the controversy. Int J Sports Med 25, 284–293.
McConnell AK & Sharpe GR (2005). The effect of inspiratory muscle training upon maximum lactate steady-state and blood lactate concentration. Eur J Appl Physiol 94, 277–284.
Romer LM & Dempsey JA (2006). Legs pay out for the cost of breathing! Physiology News 65, 25–27.
Romer LM, McConnell AK & Jones DA (2002). Effects of inspiratory muscle training on time-trial performance in trained cyclists. J Sports Sci 20, 547–562.
Volianitis S, McConnell AK, Koutedakis Y, McNaughton L, Backx K & Jones DA (2001). Inspiratory muscle training improves rowing performance. Med Sci Sports Exerc 33, 803–809.
