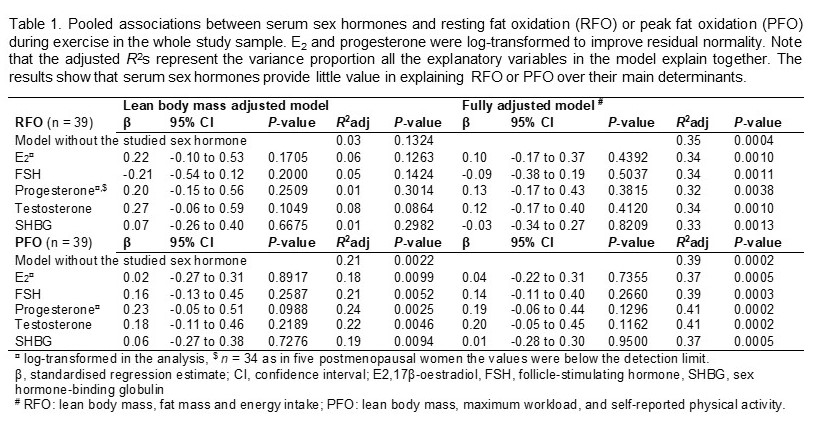
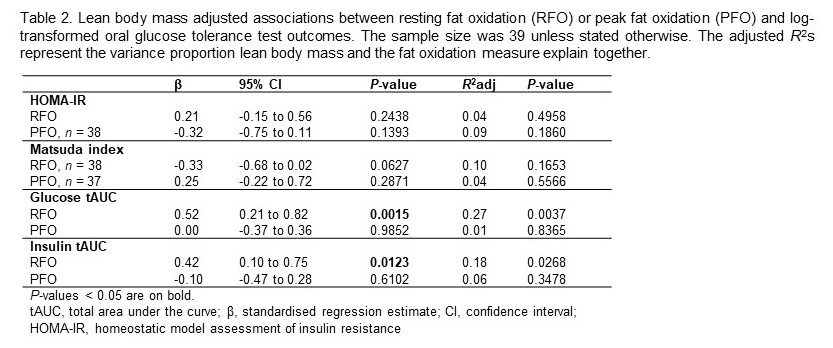
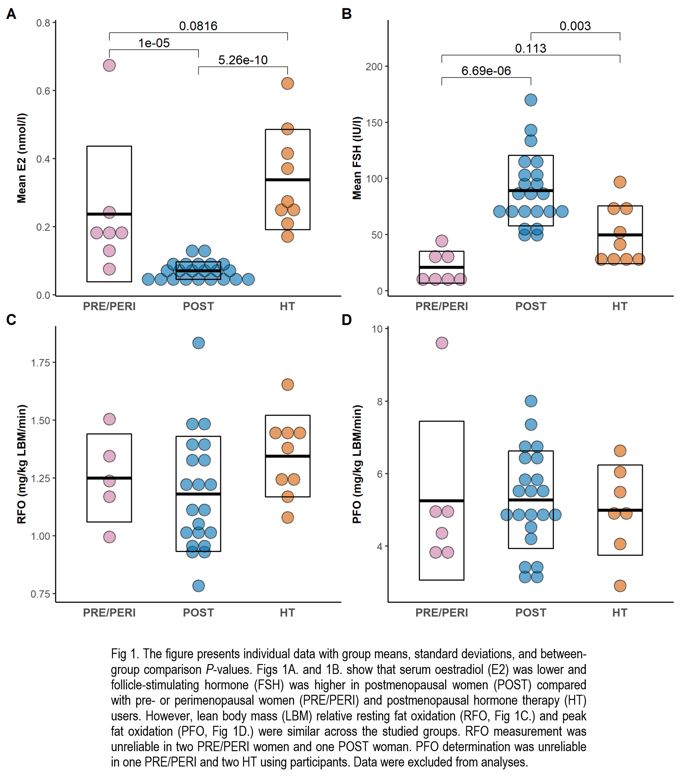
Menopause is considered to reduce whole-body fat oxidation due to systemic oestrogen deficiency. The premise is based on a few human studies, and no data exist if hormonal status explains peak fat oxidation (PFO) during exercise in middle-aged women. Menopause is linked to an increase in cardiometabolic disease incidence. One underlying mechanism could be insulin sensitivity loss due to fat oxidation capacity decline and subsequent accumulation of lipid intermediates in oxidative tissues. Ageing is often a confounder in menopause studies. Therefore, we studied if serum sex hormone profile explains resting fat oxidation (RFO) and PFO among similar age women with varying menopausal states. We also investigated associations between the fat oxidation measures and oral glucose tolerance test (OGTT) outcomes. Our sample was 42 women (mean age 55.3 [SD 1.6] years), of which seven were pre-or perimenopausal, 26 were postmenopausal, and nine were postmenopausal oestrogen-containing hormone therapy users. Four postmenopausal women were excluded from between-group comparisons due to premenopausal range oestradiol levels. We measured RFO and PFO with indirect calorimetry at separate laboratory visits. PFO was determined during a bicycle-ergometry test using four-minute stages and 20 W workload increases. Cardiorespiratory fitness, quantified as maximum workload, was then measured with a ramp protocol to voluntary exhaustion. Standard 2-h OGTT was performed after RFO measurement. Blood-based biomarkers were measured using clinical chemistry. Lean body mass (LBM) and fat mass were determined with dual-energy x-ray absorptiometry. Physical activity was assessed with a questionnaire and accelerometers. Diet was recorded with two-day food diaries before measurements. We analysed between-group differences using ANOVA with Tukey’s post hoc test and individual-level associations using multivariable linear regression. The Ethics Committee of the Central Finland Health Care District approved the study (Dnro 9U/2018). Participants gave informed consent. The menopausal groups had discordant oestradiol (F [2, 35] = 44.74, P < 0.0001) and follicle-stimulating hormone FSH (F [2, 35] = 18.24, P < 0.0001) levels but similar LBM relative RFO (F [2, 32] = 1.67, P = 0.2041) and PFO rates (F [2, 32] = 0.10, P = 0.9047) (Fig. 1). We did not observe statistically significant associations between the measured sex hormones and fat oxidation (Table 1). RFO was positively associated with fat mass (standardised regression coefficient [β] = 0.44, P = 0.0057, n = 39) and negatively with energy intake before assessment (β = -0.41, P = 0.0188, n = 39). PFO was positively associated with cardiorespiratory fitness (β = 0.59, P = 0.0019, n = 39), LBM (β = 0.48, P = 0.0022, n = 39) as well as self-reported (β = 0.41, P = 0.0116, n = 39) and accelerometery-measured physical activity (β = 0.36, P = 0.0196, n = 37). RFO was positively associated with OGTT glucose and insulin areas under the curves; however, we observed no statistically significant associations with PFO and OGTT outcomes (Table 2). In conclusion, menopause may not have a meaningful impact on RFO or PFO over their well-known determinants. Higher whole-body fat oxidation rates do not necessarily reflect better insulin sensitivity.
Physiology 2021 (2021) Proc Physiol Soc 48, PC057
Poster Communications: Systemic sex hormones do not explain resting fat oxidation or peak fat oxidation during exercise in women with varying menopausal states
Jari E. Karppinen1, Hanna-Kaarina Juppi2, Jukka Hintikka1, Petri Wiklund1, 3, 4, 5, Eero A. Haapala1, 6, Matti Hyvärinen2, Tuija Tammelin7, Pauliina Aukee8, Urho M. Kujala1, Jari Laukkanen1, 9, 10, 11, Eija K. Laakkonen2
1 Faculty of Sport and Health Sciences, University of Jyväskylä, Jyväskylä, Finland 2 Gerontology Research Center and Faculty of Sport and Health Sciences, University of Jyväskylä, Jyväskylä, Finland 3 Department of Epidemiology and Biostatistics, School of Public Health, Imperial College London, London, United Kingdom 4 Faculty of Medicine, University of Oulu, Oulu, Finland 5 The Exercise Translational Medicine Centre, Shanghai Jiao Tong University, Shanghai, China 6 Faculty of Biomedicine, University of Eastern Finland, Kuopio, Finland 7 LIKES Research Centre for Physical Activity and Health, Jyväskylä, Finland 8 Department of Obstetrics and Gynecology, Pelvic Floor Research and Therapy Unit, Central Finland Central Hospital, Jyväskylä, Finland 9 Institute of Clinical Medicine, Department of Medicine, University of Eastern Finland, Kuopio, Finland 10 Institute of Public Health and Clinical Nutrition, University of Eastern Finland, Kuopio, Finland 11 Department of Internal Medicine, Central Finland Healthcare District, Jyväskylä, Finland
View other abstracts by:
Where applicable, experiments conform with Society ethical requirements.