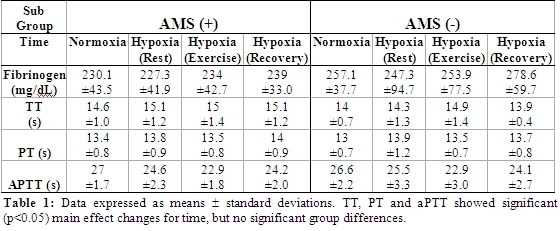
Introduction: Previous research in our laboratory has identified that the neurological components of AMS, especially headache are a potential consequence of oxidative stress. Since activation of the coagulation cascade is potentially subject to redox regulation in-vivo, the current study aimed to assess the haemostatic differences in AMS (+) and AMS (-) individuals. Methods: Following local ethical approval, and after gaining written, informed consent, 18 apparently healthy male volunteers were recruited. Subjects were assigned days to attend the laboratory to be administered 6 hours passive exposure to normobaric hypoxia (Fraction of inspired oxygen [FIO2] 12%) in an environmental chamber. After 6 hours exposure, the subjects were asked to perform an incremental cycling test to volitional exhaustion. Blood was sampled at four time points FIO2 21% [Normoxia], 6 hours passive hypoxic exposure [Hypoxia (rest)], immediately post exercise in hypoxia [Hypoxia (Exercise)] and at 8 hours exposure: [Hypoxia (Recovery)]. Blood was sampled via an in-dwelling cannula into sodium citrate vaccutainers and tested for plasma levels of Fibrinogen (FB), Prothrombin Time (PT), Thrombin Time (TT) and Activated Thromboplastine Time (aPTT) using a Futura Pluss Coagulometer. AMS was diagnosed using the Lake Louise (LL) score (clinical + self-assessment scores) of ≥5 points and an Environmental Symptoms Questionnaires (ESQ) cerebral score of ≥0.7 points at Hypoxia (Rest). Results: Clinical AMS was diagnosed in 50% of subjects. Data were corrected for plasma volume changes where appropriate i.e. fibrinogen data were corrected, but TT, PT and aPTT were not as these data represent times. No differences in plasma levels of FB, PT, TT or aPTT were discovered between sub-groups. Conclusions: Though exercise activated the coagulation cascade, as seen in significant changes in combined data for TT, PT and aPTT, the difference in response between AMS (+) and AMS (-) was not found to be significant. The alterations in vascular reactivity previously described by our group in AMS (+) cannot be ascribed to haemostatic alterations.
University of Cambridge (2008) Proc Physiol Soc 11, C10
Oral Communications: Acute mountain sickness does not alter the coagulation cascade differently in susceptible and non-susceptible individuals
L. Fall1, K. A. Evans1, P. N. Ainsle2, P. Martins1, E. Kewley1, D. M. Bailey1
1. Department of Science and Sport, University Of Glamorgan, Pontypridd, Wales, United Kingdom. 2. Department of Physiology, University of Otago, Otago, New Zealand.
View other abstracts by:
Data Table
Where applicable, experiments conform with Society ethical requirements.