Introduction
Pressure ulcers (PU) arise from localised damage to the skin through a combination of sustained pressure and shearing forces, costing ~£8 billion a year to treat in the UK(1). Microclimate conditions within and around skin tissues influence its tolerance to mechanical loading, with cooling reducing skin tissue’s metabolic demands and increasing its tolerance to mechanical damage(2). This has informed the design of several therapeutic interfaces and surfaces delivering local cooling via microclimate management systems(3). However, evidence underlying their efficacy across different populations remain limited. It is unclear whether interventions should be adjusted based on factors such as age and skin site. This knowledge gap is driven by a lack of normative data on age- and body site-dependent differences in skin epidermal properties and microvascular density, which could modulate the efficacy of localised cooling therapy for PU prevention.
The aim of this study was to characterise age- and anatomical site differences in skin epidermal thickness and microvascular density using optical coherence tomography (OCT), in younger and older adults.
Methods
Ethical approval was granted by the University of Southampton Ethics Committee (ERGO:88984). Twenty-two younger (25±4y; 71±9Kg; 17±9cm) and 19 older adults (65±4y; 70±14Kg; 171±10cm) with no health conditions, underwent an in vivo characterization of epidermal thickness (µm) and vascular density (expressed as a % of tissue comprising blood vessels against the depth of detection) at two skin sites, the sacrum and posterior heel. Skin properties were assessed using an OCT scanner. Vascular density data were analysed using a three-way ANOVA to assess the interaction between blood vessel depth, age, and anatomical site. Epidermal thickness was analysed using a two-way ANOVA to assess the interaction between age and anatomical site.
Results
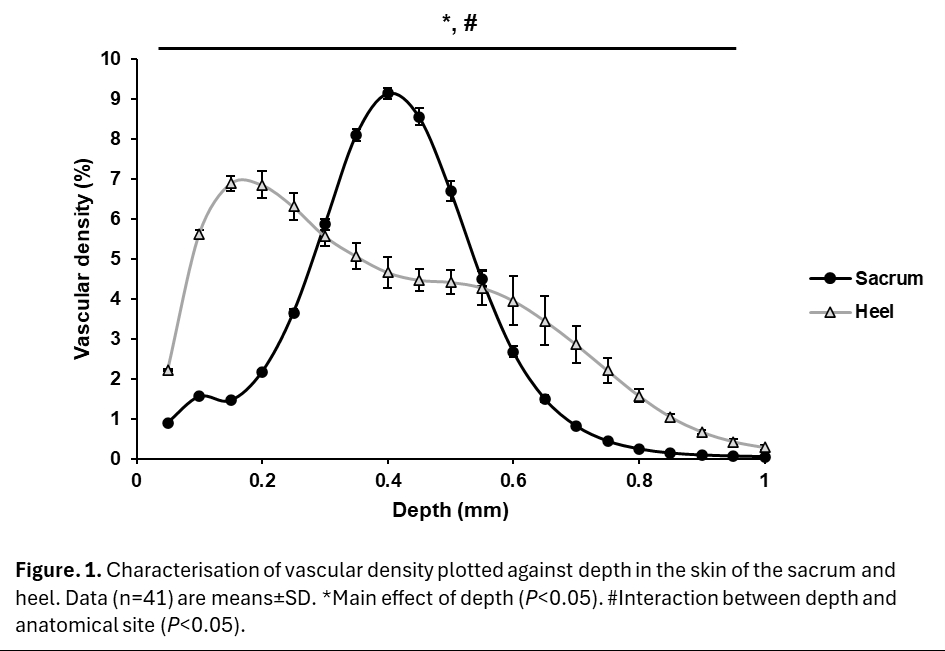
There was a main effect of depth (P<0.001) on vascular density (Fig. 1) and an interaction between depth and the anatomical site (P<0.001), but no effect of age on either depth (P=0.810) or skin site (P=0.517). Post-hoc analyses indicated that peak vascular density in the sacrum (depth 0.4mm) was greater than in the heel (mean difference +4.5%, 95%CI [3.7, 5.2], P<0.001). In contrast, peak vascular density in the heel occurred at a more superficial depth (0.15mm) and lower magnitude compared to the sacrum (mean difference -5.5%, 95%CI [-6.3, -4.7], P<0.001).
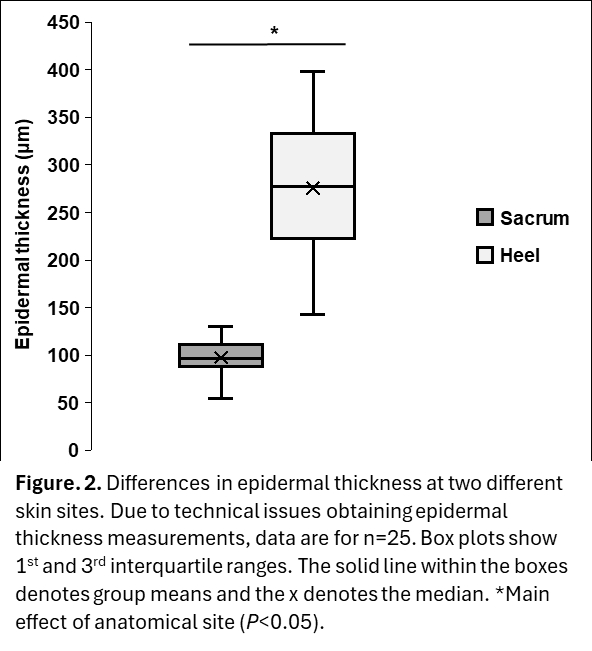
The epidermal thickness of the skin was greater in the heel than the sacrum (mean difference +180.9µm, 95%CI [156.6, 205.4], P<0.001, Fig. 2), but there was no effect of age between younger and older groups (P=0.388).
Conclusions
Results highlighted an effect of body site, but not age, in skin epidermal properties and microvascular density across two skin regions at risk of PU development. The heel presented a thicker epidermis, and a lower absolute and more superficial microvascular density than the sacrum, which presented a thinner epidermis and higher and deeper microvascular density. Importantly, ageing did not clearly alter the tested skin properties. Altogether, these findings indicated that localised thermal intervention may need to consider variations in epidermal and vascular properties with skin site to optimise the efficacy of skin cooling in maintaining skin tissue viability.