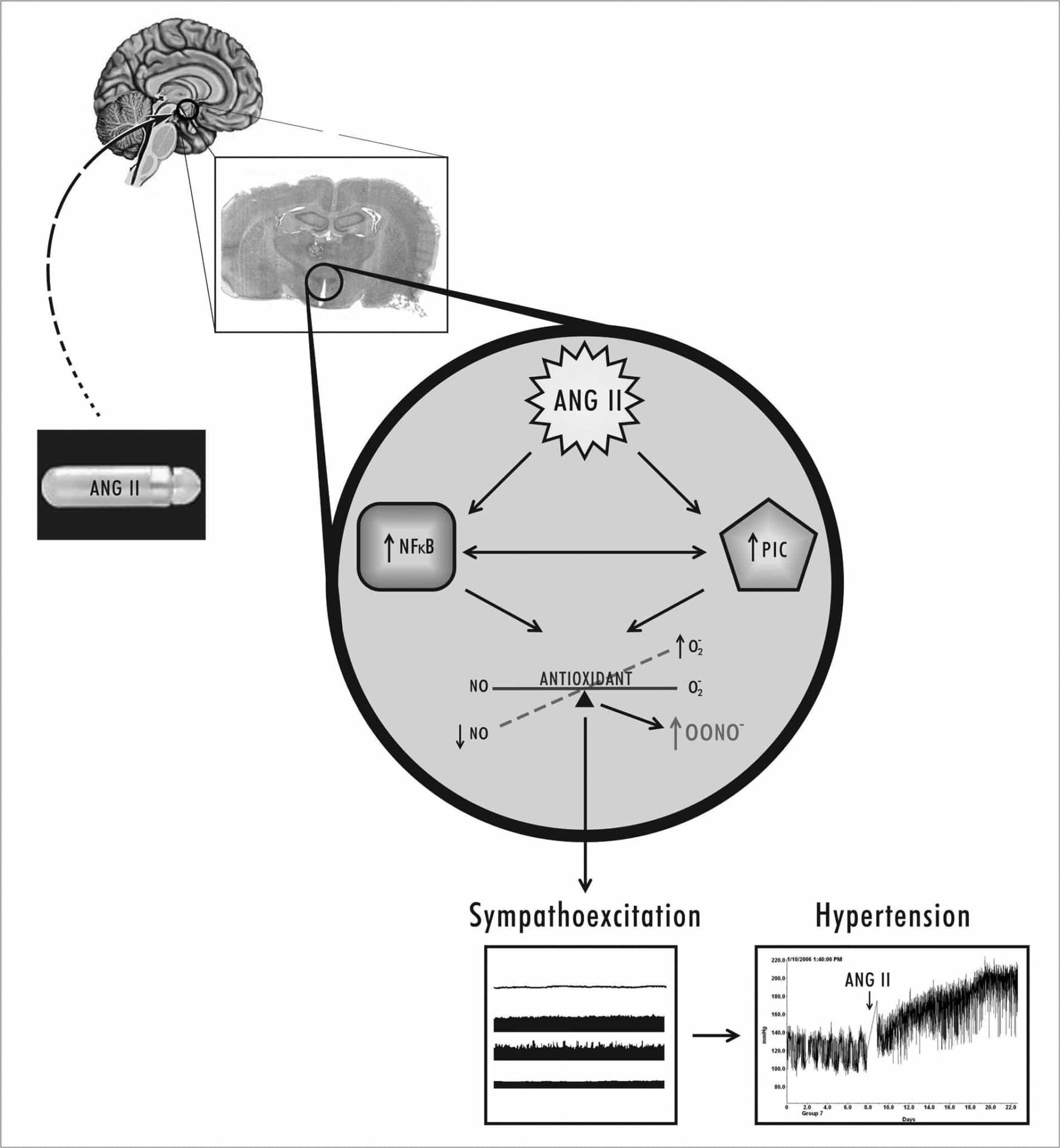
Hypertension is the single most important predisposing factor for the development of cardiovascular and renal impairments. It is estimated that 15 to 20% of the global adult population suffers from hypertension; however, the etiologies of 95% of essential hypertension cases are not known1. Interestingly, about 65% of patients with essential hypertension respond to angiotensin converting enzyme inhibitors and angiotensin receptor blockers, suggesting that angiotensin plays a pivotal role in essential hypertension. Several prospective clinical trials have found calcium channel antagonists and angiotensin receptor blockers to be efficient in treating hypertension; however, the clinical course of hypertension is progressive, often leading to stroke, heart failure and renal damage. Consequently, new and innovative approaches for treating hypertension are needed. Although hypertension is a disease of the blood vessels, recent evidence suggests that the central nervous system plays an important role in the onset and development of hypertension. More importantly, hypertensive patients and animals have increased sympathetic activity, accompanied by alterations in body fluid homeostasis. In the brain, the paraventricular nucleus (PVN) of the hypothalamus plays an important role in regulating sympathetic drive, blood pressure (BP) and body fluid homeostasis2. Interestingly, levels of angiotensin (ANGII), and its receptor (AT-1R), are upregulated in the PVN in hypertensive animals. Injection of ANGII acutely or chronically induces a pressor response which is accompanied by increased sympathetic nerve activity. Blockade of ANGII in the brain attenuates the hypertensive response and decreases sympathetic activity, suggesting that the PVN plays an important role in the regulating BP and sympathetic activity. In addition to neurohormones, proinflammatory cytokines (PIC), such as tumor necrosis factor (TNF-α), are increased in the circulation in cardiovascular disease and are of prognostic significance. Previously we reported that cytokines are not only increased in the circulation, but also in the brain, particularly in the PVN of the hypothalamus. We also demonstrated a role for cardiac sympathetic afferents in the activation of cytokines in the brain. One of the most important downstream molecules involved in the activation of PIC is nuclear transcription factor kappa B (NFκB). NFκB is not only involved in production of PIC, but also in the induction of oxidative and nitrosative stress. However, it is not known whether NFκB or PIC in the PVN contribute to the development of high BP. Recent studies from our laboratory suggest that: 1) cytokines and NFκB are activated in the PVN of rats with heart failure4 and hypertension5; 2) blockade of cytokines or of NFκB within the central nervous system attenuates hypertensive response in ANGII infusion models5; 3) cytokines in the brain modulate the major reactive oxygen species (ROS) molecules, such as superoxide and nitric oxide (NO), in the PVN, and contribute to heart failure6; and 4) mice lacking the gene for TNF-α have no response to ANGII infusion7. These findings suggest an important central nervous system role for inflammatory molecules in cardiovascular disease. The overall objective of our research is to determine the roles played by inflammatory molecules in the regulation of cardiovascular function. In this presentation, we will examine the roles played by cytokines and transcriptionally active NFkB in the PVN in an ANGII infusion model of hypertension and their contributions to sympathoexcitation (Figure 1). We will chronically infuse ANGII in rats and mice and examine the roles played by cytokines and NFkB in the progression of hypertension. Mouse models are used to delineate the roles played by NFkB and TNF in ANGII-induced hypertension. We will use a comprehensive, whole animal, molecular, cellular and genetic approach to explore the possible mechanisms by which cytokines or NFkB in the PVN modulate sympathoexcitation and contribute to the progression of the disease. Finally, we will also present data on the effect of direct manipulation of PVN cytokines or NFkB in the development of hypertension. Some of our findings will suggest that cytokine- or NFkB-induced neurohumoral excitation plays an important role in the pathogenesis of hypertension. The central link between cytokines and the neurohumoral system, which are activated in hypertension, may lead to a better understanding of the progression of the disease process and ultimately lead to new and effective strategies to treat hypertension.
University College Dublin (2009) Proc Physiol Soc 15, SA37
Research Symposium: Central nervous system cytokines in hypertension
J. Francis1
1. Comparative Biomedical Sciences, Louisiana State University, Baton Rouge, Louisiana, USA.
View other abstracts by:
Where applicable, experiments conform with Society ethical requirements.