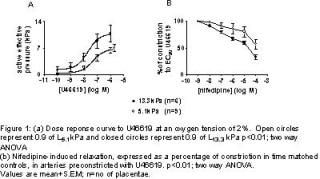
Normal fetal development depends on adequate blood flow to the placenta. Regulation of fetoplacental blood flow has been examined in the perfused organ in vitro and in this model reducing oxygen tension raises perfusion pressure although the mechanisms are poorly understood. Hypertension has also been shown to enhance the vascular response to vasoconstrictors in rat pulmonary arteries (Thomas and Wanstall 2003). Here we examine (a)the interaction between oxygen tension and normalisation pressure on U46619-(thromboxane mimetic) induced constriction of isolated placental chorionic plate arteries, and (b)the effect of nifedipine, an L-type voltage-gated Ca2+ channel blocker.Term placentae were obtained from uncomplicated pregnancies with written consent. Chorionic plate arteries (diameter=283±14µm) were mounted and normalised at a pressure equivalent to 0.9 of kPa or 0.9 of L13.3 kPa, on a wire myograph as described L5.1 previously (Wareing et al 2002). Vessels were then equilibrated for 30 min in physiological salt solution gassed with 5% or 2% oxygen. Constriction to U46619 (10-10-10-6M) was performed, paired vessels were then pre-constricted to U46619 (EC80) and the effect of incremental doses of nifedipine (10-8-10-4M) or DMSO (diluent) assessed.At 5% oxygen and vessel normalisation to 0.9 of L5.1 kPa, U46619 induced a constriction of 7.5±1kPa (n=4 placentae). Increased normalisation pressure did not affect the magnitude of constriction (9.1±3kPa n=4). The U46619-induced constriction at 0.9 of L5.1 kPa was partially inhibited by 10-4M nifedipine (residual constriction=45.4±10%) indicating that nifedipine-sensitive and -insensitive mechanisms contribute to U46619-induced constriction. Increasing normalisation pressure did not affect the nifedipine relaxation (residual constriction=48.2±7%).At 2% oxygen and vessel normalisation of 0.9 of L5.1 kPa, U46619-induced a constriction of 6.8±0.7kPa, this was raised significantly when the normalisation pressure was increased (10.9±2.2; figure 1A). At 0.9 of L5.1 kPa the U46619induced constriction was partially inhibited by 10-4M nifedipine (residual constriction=57.7±9%). Increasing the normalisation pressure significantly increased the relaxation in response to nifedipine (residual constriction=33.3±5%; figure 1B). These studies demonstrate that low oxygen tension increases (i)the constriction to U46619 and (ii)relaxation to nifedipine in placental arteries normalised at 0.9 of L13.3 kPa but not at 0.9 of LkPa. We propose that nifedipine-sensitive Ca2+ channels have a role in mediating the raised vasoconstrictor response to U46619 under conditions of low oxygen tension and raised vascular pressure.
University of Glasgow (2004) J Physiol 557P, PC36
Communications: Effect of oxygen tension and pressure on the vascular responses of human placental chorionic plate arteries.
E.J. Cooper, M. Wareing, P.N. Baker and S.L. Greenwood Maternal and Fetal Health Research Centre, University of Manchester, Manchester, UK
Maternal and Fetal Health Research Centre, University of Manchester, Manchester, UK
View other abstracts by:
Where applicable, experiments conform with Society ethical requirements.