Fibroblasts form one of the largest cell populations in the heart (Fig. 1), outnumbering cardiomyocytes in healthy myocardium by a factor of at least two [1]. The relative proportion of fibroblasts in the heart increases with age, and shows pronounced regional differences. Cardiac pacemaker and conduction tissue, for example, has a high connective tissue content even under physiological conditions, as highlighted by Arthur Keith and Martin Flack in 1906: ‘Purkinje fibres […] are isolated from the rest of the musculature […] by well-developed connective-tissue sheaths’ [2]. Many pathological conditions cause further fibroblast proliferation and/or invasion, and give rise to either diffuse (fibrosis) or localized (scarring) elevation in connective tissue content. As apparent from the quote above, and somewhat paradoxically given its name, connective tissue in the heart was and is usually assumed to form a barrier, i.e. to divide. This has also dominated the view on its role in cardiac electrophysiology, even though isolated fibroblasts and myocytes show abundant heterogeneous coupling in vitro, as has been seen from the very beginning of cardiac cell culture work [3]. Assessment of fibroblast-myocyte electrical interaction in situ is not as straightforward as it may seem, since i) cardiac fibroblasts have a very high membrane resistance (109-1010 Ohm), and ii) they form very long sheet-like processes in native tissue [4]. This means that i) it is nearly impossible to identify individual fibroblast-myocyte coupling in native tissue by micro-electrophysiological means (as any myocyte-coupled fibroblast will simply follow the myocyte’s trans-membrane potential changes, including mimicry of action potential waveforms), while isolation of intact fibroblast-myocyte pairs, or complete individual fibroblasts, is difficult (due to the spatial extent of fibroblasts, which will cause truncation during the process of tissue digestion, mincing, and agitation for cell release). Alternative experimental approaches include i) the use of dyes to study heterogeneous cell coupling in intact tissue, or ii) the mapping of electrical propagation in cardiac scars. Both methods have provided clear evidence for heterogeneous fibroblast-myocyte coupling [5, 6]. The probable substrate for this interaction has been identified in native rabbit sino-atrial node as small gap junctions connecting the different cell population [5]. Electrophysiological consequences of myocyte-fibroblast electrotonic interaction have been studied in ‘wet’ [7] and ‘dry’ model systems [8]. They suggest that – in addition to forming obstacles to electrical conductions – fibroblasts could act as i) passive electrotonic loads / current sinks or, ii) if bridging gaps between myocyte groups as conductors of excitation. In situ, this could affect crucial electrophysiological parameters such as excitability, refractoriness and electrical load (which are key determinants of arrhtythmogenic tissue properties), and/or provide conduction pathways outside the traditional conceptual framework of myocyte-myocyte only coupling, such as seen in cases of donor-recipient cardiac coupling across transplantation scars (which occurs in about 10% of human heart transplants), or with electrical invasion of post-infarct scar tissue [6]. This possibility has triggered investigations into the potential of genetically modified fibroblasts to act as modulators of cardiac automaticity [9], and it may form an interesting, if unconventional, target for anti-arrhythmic drug actions [10]. Thus, cardiac fibroblasts contribute to cardiac electrophysiology, apparently assuming roles beyond the formation of passive obstacles, by acting as current sinks and/or electrical conduction pathways. Details of in situ myocyte-fibroblast interaction in different regions of the heart, and the mechanisms that govern regulation of heterogeneous cell interaction in health and disease, are still ill-explored, and form a potentially exciting target for further research.
University of Manchester (2007) Proc Physiol Soc 8, SA22
Research Symposium: Fibroblasts and cardiac electrophysiology
P. Camelliti1, P. Kohl1
1. Physiology, Anatomy & Genetics, University of Oxford, Oxford, United Kingdom.
View other abstracts by:
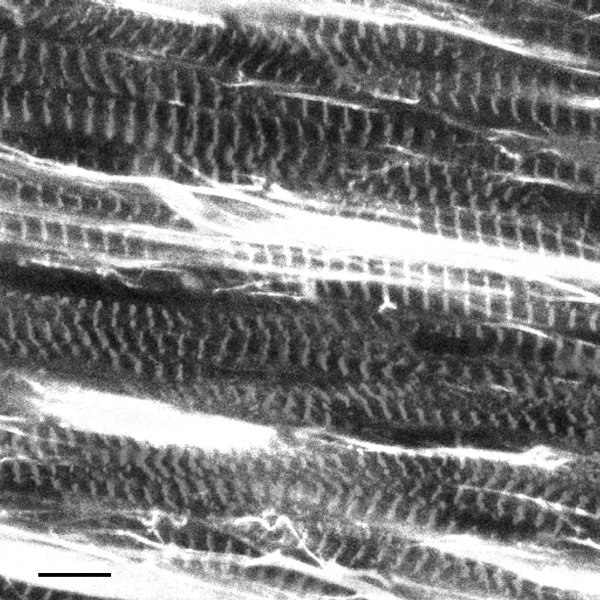
Figure 1: Confocal micrograph of rabbit right atrial myocardium, immunohistochemically labelled for cardiomyocytes (myomesin label, giving rise to striated cell appearance) and fibroblasts (vimentin, revealing brightly stained cell sheets between myocytes). Scale bar 10 μm.
Where applicable, experiments conform with Society ethical requirements.