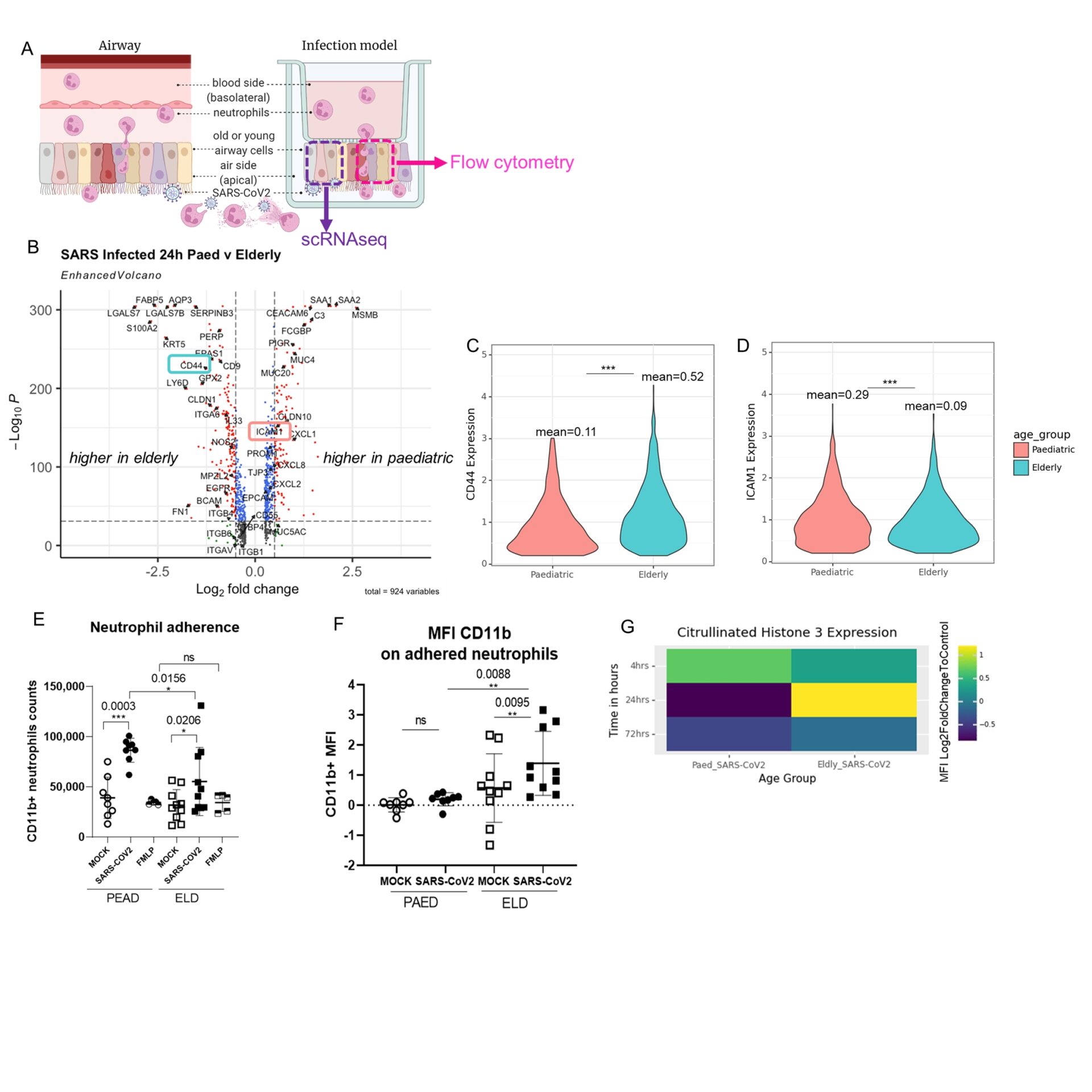
BACKGROUND: The COVID-19 pandemic caused by the SARS-CoV-2 virus has resulted in over 6.5 million deaths, predominantly in the elderly (Huang et al., 2020). There is little understanding regarding how COVID-19 severity increases with age. Neutrophils are found in large numbers in the airways of the lungs in severe COVID-19 patients (Veras et al.,2020) We aim to understand whether this influx of neutrophils into the airway has a protective or detrimental effect. To do this we investigated the function of neutrophils during SARS-CoV-2 infection and their interaction with the airway epithelium using an experimental infection model of the airway epithelium from children and the elderly (Figure 1A).
METHODS: Nasal airway cells obtained from healthy elderly (>70y) and young (<11y) individuals (n=18 total: elderly n=10, paediatric n=8) were differentiated at air-liquid interface as described before (Woodall M et al., 2021). Epithelial cells were then infected with SARS-CoV-2 for 24h. Airway epithelial cells were subsequently analysed by single-cell RNA sequencing (scRNAseq) (Figure 1A) to identify differentially expressed genes that could impact neutrophil migration (Figure 1B). To test this functionally, human neutrophils were added to the basolateral (blood) side of infected epithelial cells so that they migrate to the apical (air) and infected side of the epithelium, similar to a physiological airway (Figure 1A). Neutrophils were then recovered after 1h for flow cytometric analyses (Figure 1A).
RESULTS: scRNAseq data showed that CD44; a glycoprotein expressed on the surface of both the airway epithelium and neutrophils; was highly expressed in the elderly airway epithelium 24hrs post SARS-CoV-2 infection (Figure 1B,C). Whilst ICAM-1 is more highly expressed in the paediatric epithelium (Figure 1B,D). We also found higher numbers of neutrophils adhered to SARS-CoV-2 infected paediatric epithelium compared to SARS-CoV-2 infected elderly epithelium (Figure 1D). In addition we found increased activation of neutrophils (CD11b+) (Figure 1F) and more Citrullinated Histone 3 positive neutrophils (Figure 1G) migrated across the SARS-CoV-2 infected elderly compared to the paediatric epithelium.
CONCLUSION: Our data suggest that neutrophils have a weaker and less stable adhesion to SARS-CoV-2 infected nasal epithelium with increasing age. This may be due to the interaction of LFA-1 on neutrophils and ICAM-1 on the SARS-CoV-2 paediatric airway which is mediated by stronger electrostatic and hydrophobic forces. Whereas the interaction between CD44 on the elderly airway epithelium and neutrophils is facilitated by hyaluronic acid, a polysaccharide of which their binding affinity can vary depending on inflammation. Overall, these findings point to an inflammatory neutrophil phenotype influenced by an elderly epithelium and supports the hypothesis that neutrophils contribute to COVID-19 severity.