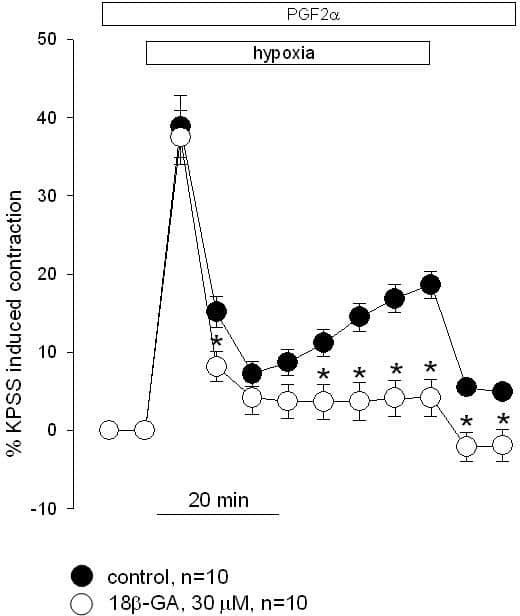
Hypoxia causes pulmonary artery constriction normally maintaining optimal ventilation-perfusion matching in the lung, but leading to pulmonary hypertension development. Although it is known that sustained hypoxic pulmonary vasoconstriction (HPV) is critically dependent on both the endothelium and glycolysis, the signaling pathways remain unclear. The aim of this study was to determine the role of gap junctions in HPV, and specifically to test the hypothesis that signaling via these junctions contributes to the sustained phase of HPV. Vascular tone was measured on rat small intrapulmonary arteries (IPA) using a wire myograph technique. In vivo experiments were performed on rats with retrograde catheterization of the right ventricle and the left common carotid artery for systolic right ventricular pressure (RVP) and mean arterial pressure (MAP) registration. Animals were anesthetized with chloralose/urethane (80 and 800 mg/kg respectively).Hypoxia (PO2 2-3 mmHg) elicited a biphasic response in tension in IPA preconstricted with prostaglandin F2α (3 µM). The transient phase I of HPV reached 39±4% of the maximum contraction elicited with 80 mM K+ (TK) (n=10), and the sustained HPV phase II reached a level of 19±2% TK (n=10). The gap junction inhibitor 18β-glycyrrhetinic acid (18β-GA, 30 µM) had no effect on HPV transient phase (37±3% TK, n=10, P>0.05) but abolished sustained HPV (4±2% TK, n=10, P<0.05). Further elevation in 18β-GA concentration to 60 and 100 µM led to significant suppression of both HPV phases. In IPA precontracted with 25 mM K+ 18β-GA (30 µM) also inhibited HPV phase II (2±2%, n=7 vs. 13±2% TK in control, n=7, P<0.05) but had no effect on phase I (22±3% TK, n=7 vs. 25±3% TK in control, n=7, P>0.05). In in vivo experiments hypoxia resulted in a biphasic increase in RVP, consisting of transient and sustained phases. RVP increased from 29.7±1.1 to 41.8±1.3 mmHg (n=10, P<0.001) in the first phase and to 40.4±1.3 mmHg (n=10, P<0.001) in the phase II. In animals treated orally with 18β-GA (25 mg/kg) 20 hours before the experiment a slight inhibition of the transient phase (33.2±4.3 mmHg, n=5, P>0.05) and complete abolition of the sustained RVP increase (27.1±1.9 mmHg, n=5, P<0.001) were observed. Hypoxia also induced systemic arterial hypotension. MAP decreased during 15 min. of hypoxia from 101.5±5.3 to 63.6±5.1 mmHg (n=10, P<0.001). The initial MAP values were significantly higher in animals treated with 18β-GA (120.5±4.5 mmHg, n=5, P<0.05) but there was no difference in MAP values during hypoxia (67.0±8.2 mmHg, n=5, P>0.05). Taken together, these data indicate that gap junctions are involved in HPV development, reflecting a novel pathway for signalling during hypoxia in pulmonary artery that supports the sustained phase of HPV.
University of Manchester (2010) Proc Physiol Soc 19, PC89
Poster Communications: Inhibition of gap junctions abolishes sustained phase of hypoxic pulmonary vasoconstriction
I. V. Kizub1,2, E. V. Strelkov1, A. I. Soloviev1, P. I. Aaronson2, J. P. Ward2
1. Experimental Therapeutics, Institute of Pharmacology and Toxicology of Academy of Medical Sciences of Ukraine, Kiev, Ukraine. 2. Asthma, Allergy, and Lung Biology, King?ÇÖs College London, London, United Kingdom.
View other abstracts by:
The effect of gap junctions inhibition with 18β-glycyrrhetinic acid (18β-GA) on HPV in rat IPA precontracted with 3 µM PGF2α. * - P < 0.05.
Where applicable, experiments conform with Society ethical requirements.