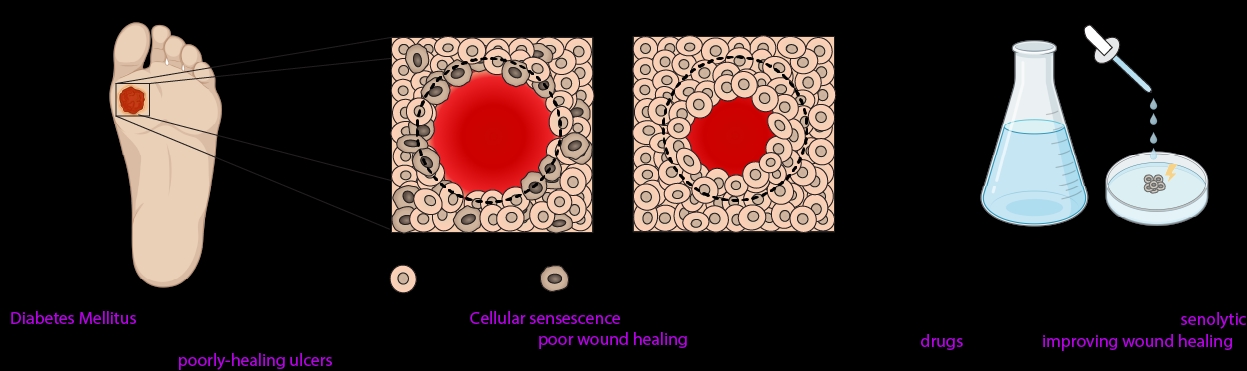
Diabetes Mellitus (DM) is a lifelong condition characterised by persistent hyperglycaemia due to insulin resistance or impaired insulin production (1). DM causes a wide array of complications, including peripheral neuropathy, which can result in the development of neuropathic ulcers. These ulcers substantially increase infection risk, resulting in further morbidity, and pose significant psychosocial challenges to suffers of DM (2). Current treatments are inadequate, with healing taking place over months to years, and not at all in some patients (3). Therefore, further understanding of the factors that regulate poor healing is required to develop more adequate therapies. It has been suggested that senescent cells could play a role in wound healing (4). Thus, combating senescence using senescence-targeting (senolytic) drugs may have a beneficial effect on wound healing. We therefore set out to test the healing-promoting effects of two senolytics, metformin and rapamycin, using a human ex-vivo skin wounding model.
Human skin samples were collected post-surgery, with full informed and written patient consent, from Castle Hill Hospital with no other inclusion criteria. Skin was washed and 2mm wounds were created using a biopsy punch. A 6mm biopsy punch was then used to cut out a 6mm explant around each wound, with the 2mm wounds lying centrally within the explants. Metformin and Rapamycin were diluted in dimethyl sulfoxide (DMSO) to a working concentration of 62.5nM and 12.5nM respectively with 2μL of treatment applied topically to wounds. 0.1% DMSO was used as a control treatment. Wounds were incubated in a humidified incubator at 32-37°C and 5% CO2 for 2 days. Wound explants were fixed and immunofluorescence staining was conducted with a primary Keratin-14 antibody followed by a secondary antibody (AlexaFluor488). Wounds were counter-stained with DAPI and images were acquired using confocal microscopy. Images were analysed using ImageJ. The edge of the wound and non-healed area was drawn around using the freehand tool and the percentage of the original wound area that had healed was calculated for each wound. Significance testing was conducted with ANOVA when there was 3 or more groups, or an unpaired T test for pairwise comparisons.
There was no overall difference found in percentage wound closure when comparing vehicle treatment (DMSO) to Metformin or Rapamycin (n=67; p=0.71). To further investigate, data was stratified into subgroups based on the patient origin of the skin. After stratification, a significant difference was found between the treatment groups for patient 2 (n= 12; p=0.047) but not patients 1 (n=24; p=0.38) and 3 (n=31; p=0.27). Further testing concluded that wound closure with Rapamycin was significantly greater than the control group (p=0.03) in patient 2. The findings suggests that rapamycin has potential efficacy in wound-healing, but that such efficacy is patient-specific. This therefore warrants further investigation and testing of rapamycin on further samples from more patients.