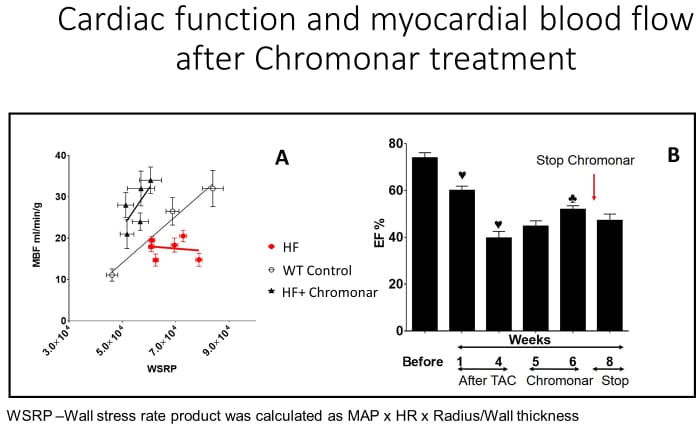
Heart failure (HF) is the leading cause of death in the US and worldwide. Current therapies have produced some measure of success in patient outcomes, but they only slow the progression of the disease. We speculate that if the correct “lesion” was targeted by the therapy, the progression could be stopped and perhaps, reversed. Coronary microvascular disease is associated with heart failure, but whether dysfunction of the coronary microcirculation causes the disease is unknown. Thus, we hypothesize the cause of heart failure is insufficient myocardial blood flow (MBF) that fails to meet the needs of the heart. The flow insufficiency produces minute areas of ischemia, resulting myocyte loss, and fibrosis with the accumulation of these events eventually leading to failure. To test this, we determined the relationship between MBF and cardiac work (wall stress-rate product [WSRP]). We examined 3 groups of animals: Group 1: control C57Bl6/J mice (CTRL); Group 2: mice with transaortic constriction (TAC) to produce HF; and Group 3: HF mice treated with the coronary vasodilator, Chromonar (4 weeks of treatment). This latter treatment was devised to show proof of principle, i.e., if flow were increased in the failing heart, would the failure be reversed? Transthoracic echocardiography was used for weekly cardiac function measurements. MBF and WSRP were measured during norepinephrine-induced increases in WSRP in anesthetized mice to create the relationship between MBF and cardiac work. The figure (Panel A) shows the relationship between WSRP and MBF in the 3 groups. Note the relationship between WSRP and MBF is uncoupled in HF, i.e., when work increases MBF does not. Moreover, Chromonar recoupled work with MBF and increased MBF (increased MBF per unit of work). These changes in flow paralleled cardiac function in the HF and HF+Chromonar groups. After TAC cardiac function decreased over 13 weeks: ejection fraction (EF) of about 40% in both groups (panel B). Chromonar treatment increased EF to 67±3%; whereas in untreated mice EF remained low. Based on these findings, we propose that a cause of HF is inadequate MBF to meet the metabolic demands of the working heart. Pharmacological coronary vasodilation with Chromonar to increase MBF in HF can reverse the functional decline and improve cardiac function.
Physiology 2019 (Aberdeen, UK) (2019) Proc Physiol Soc 43, SA026
Research Symposium: Is heart failure a coronary microvascular disorder?
V. Ohanyan1, T. Hakobyan1, L. Shockling1, T. Gyulkhasyan1, M. Enrick1, C. L. Kolz1, W. M. Chilian1
1. IMS, Northeast Ohio Medical University, Rootstown, Ohio, United States.
View other abstracts by:
Where applicable, experiments conform with Society ethical requirements.