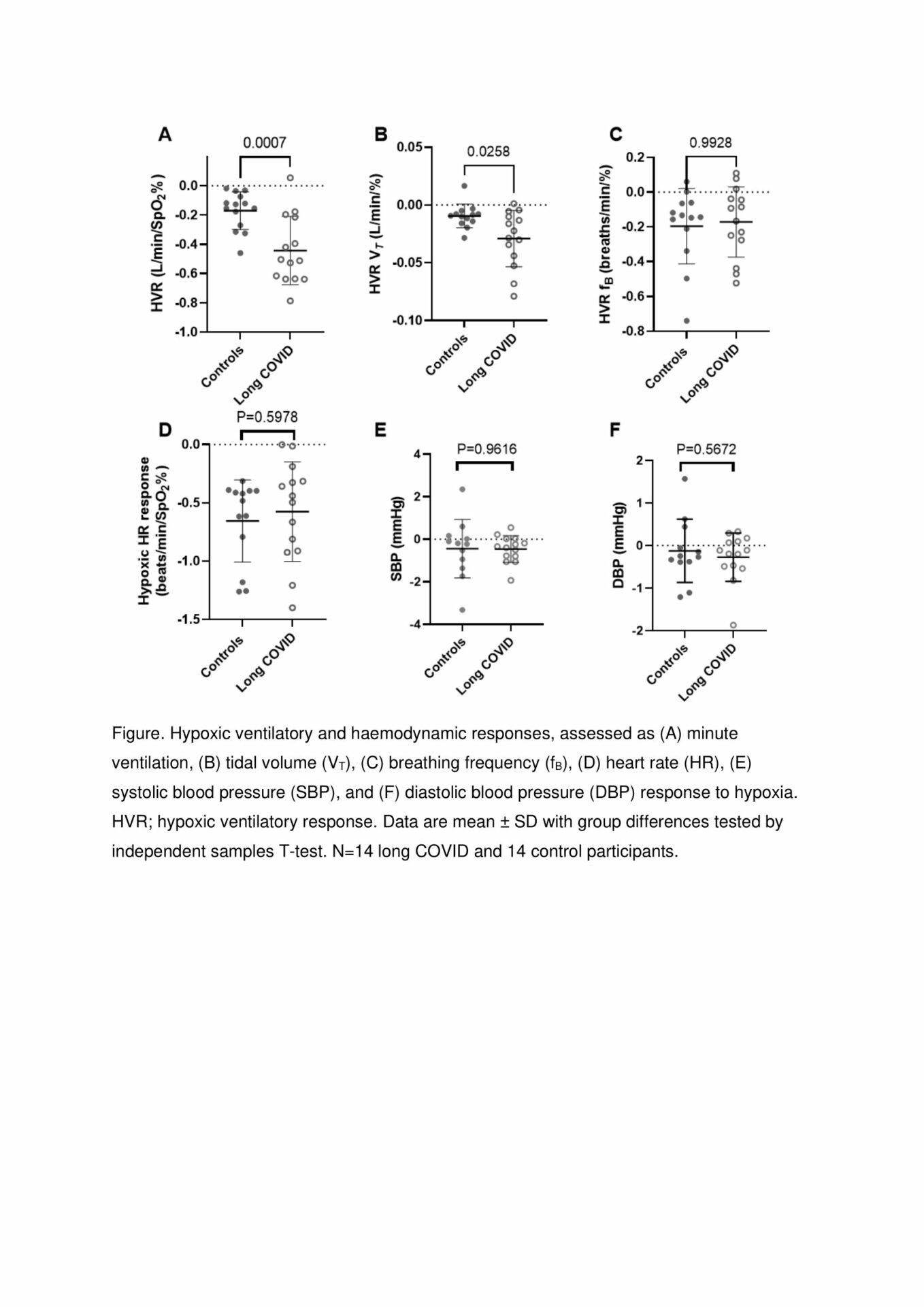
Post-COVID-19 syndrome (long COVID) describes ongoing symptoms for 12 or more weeks following infection with SARS-CoV-2. Respiratory-related symptoms including breathlessness [1], exercise intolerance and ventilatory dysfunction [2] are common in long COVID. Further, cells at the primary site of oxygen sensing (carotid bodies) are susceptible to SARS-CoV-2 infection [3]. We aimed to determine whether long COVID patients have altered carotid chemoreceptor sensitivity, by assessing resting hypoxic ventilatory response and ventilatory efficiency during exercise. Fourteen long COVID patients (3 male, 42 ± 12 years) and eight control participants (did not develop long COVID post-infection) gave written informed consent to participate in an ethically approved study (NHS REC). The control group was supplemented by six healthy individuals who undertook the same experimental procedures in the same laboratory, prior to the pandemic (in total; 2 male, 35 ± 13 years, P=0.1195 for age versus patient group). Participants did not have pre-existing respiratory or cardiovascular disease and resting lung function (spirometry) was similar between the groups. Transient hypoxia was achieved by supplementing inspired air with 100% N2 for 5-8 short periods, lasting 5-30 seconds, reducing SPO2 to nadirs of between 65 and 99%. Breath-by-breath minute ventilation (VE), tidal volume and breathing frequency, and beat-to-beat heart rate and blood pressure, were monitored during N2 supplementation and for one minute afterwards. The 95th percentile of these variables and the nadir SPO2 were determined for each hypoxic period and entered into a simple linear regression, where the slope defined response to hypoxia (peripheral chemoreceptor sensitivity). The VE response to hypoxia was greater in long COVID patients versus controls (-0.44 ± 0.23 versus -0.17 ± 0.13 L/min/SPO2, Figure; P=0.0007, independent samples T-test), demonstrating greater ventilation for a given fall in SPO2. This difference was caused by a larger tidal volume response, as breathing frequency response was similar. Heart rate and blood pressure responses were also unchanged (Figure). Participants performed a maximal exercise test (upright cycle ergometer, ramp protocol to volitional exhaustion). Long COVID patients had a lower peak VO2 versus controls (18.6 ± 4.7 versus 26.7 ± 7.4 ml/kg/min, P=0.0015), despite reaching a similar peak VE (66.4 ± 22.4 versus 71.5 ± 29.2 L/min, P=0.6012), respiratory exchange ratio (1.27 ± 0.09 versus 1.28 ± 0.11, P=0.7483), and percentage of predicted heart rate (92 ± 9 versus 97 ± 6 %, P=0.1326) to the control group. VE/VCO2 slope (ventilation for a given expired CO2 volume) was greater in the long COVID group versus controls (37.8 ± 4.4 versus 31.4 ± 4.8, P=0.0008), indicating reduced ventilatory efficiency in the long COVID group. Furthermore, VE/VCO2 slope was correlated with hypoxic ventilatory response, such that enhanced chemoreflex sensitivity was associated with poorer ventilatory efficiency during exercise (r=0.54, P=0.0037, Pearson’s correlation, n=28). These data demonstrate that long COVID is associated with high peripheral chemoreflex sensitivity and reduced ventilatory efficiency during exercise. These changes could underlie the respiratory symptoms of long COVID such as dyspnoea and exercise intolerance. Targeting the carotid body to reduce its sensitivity may provide benefit to long COVID patients.
Physiology 2023 (Harrogate, UK) (2023) Proc Physiol Soc 54, PCA039
Poster Communications: Peripheral chemoreceptor sensitivity is elevated in patients with long COVID
Zoe H. Adams1, Hazel C. Blythe1, Ahmed El-Medany1, Katrina A. Hope1, Adrian H. Kendrick1, Ana P. Abdala Sheikh1, Julian F. R. Paton1, Angus K. Nightingale1, Emma C. Ha
1School of Physiology, Pharmacology & Neuroscience, University of Bristol Bristol United Kingdom, 2Department of Cardiology, Southmead Hospital, North Bristol NHS Trust Bristol United Kingdom, 3Department of Anaesthetics, Southmead Hospital, North Bristol NHS Trust Bristol United Kingdom, 4Department of Respiratory Medicine, University Hospitals Bristol and Weston NHS Foundation Trust Bristol United Kingdom, 5Manaaki Manawa, The Centre for Heart Research, University of Auckland Auckland New Zealand, 6Bristol Heart Institute, University Hospitals Bristol and Weston NHS Foundation Trust Bristol United Kingdom,
View other abstracts by:
Where applicable, experiments conform with Society ethical requirements.