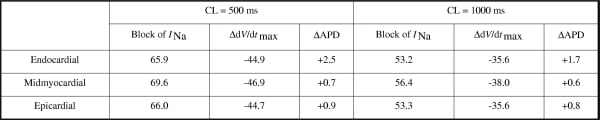
Ventricular tachycardia and fibrillation are dangerous cardiac arrhythmias. Anti-arrhythmic drugs such as lidocaine (a class 1b drug) can prevent such arrhythmias, but they have pro-arrhythmic side effects whose mechanisms are poorly understood. We used computational models to elucidate these mechanisms. Effects of lidocaine were simulated (1) in human ventricular cell models (2). The drug binds to the inactivated state of the sodium channel and has on and off rate constants of 31.0 /mM/s and 0.79 /s respectively, as measured experimentally in human ventricular cells (3). These drug effects were incorporated into 75 mm one-dimensional (1-D) heterogeneous transmural, and 12×12 cm two-dimensional (2-D) epicardial, virtual tissues (4). Drug effects were characterised and validated in single cell models. Simulated application of 0.08 mM lidocaine produced rate-dependent steady state (end systolic) block of the sodium current INa and reductions in maximum action potential upstroke velocity dV/dtmax (Table 1). There was little effect on action potential duration (APD). This is consistent with (5). In 1-D tissues, the reduced upstroke velocity under drug conditions caused reduced conduction velocity, and propagation block at short cycle lengths (CLs). The reduced conduction velocity was associated with an increased vulnerable window for unidirectional propagation (4). The maximum temporal width of the vulnerable window, expressed as a percentage of the diastolic interval, increased with pacing rate and simulated drug concentration, from 1% at CL = 1000 ms with 0.015 mM lidocaine to 18% at CL = 500 ms with 0.2 mM lidocaine. In 2-D virtual tissues, this reduced conduction velocity prevented initiation of re-entry (tachycardia), prevented breakdown of re-entry into fibrillation, or shortened the lifetime of re-entry, depending on simulated drug concentration. We conclude that the anti-arrhythmic mechanism of class Ib drugs in the virtual tissues is reduced conduction velocity, and propagation block at the high rates of excitation seen during arrhythmias. The pro-arrhythmic mechanism is an increase in the vulnerable window for unidirectional propagation, also caused by the reduced conduction velocity.
University of Manchester (2007) Proc Physiol Soc 8, PC9
Poster Communications: Reduced conduction velocity caused by class Ib anti-arrhythmic drugs contributes to both their anti- and pro-arrhythmic effects in human virtual ventricular tissues
J. A. Lawrenson1, A. P. Benson2, A. V. Holden2
1. School of Medicine, University of Leeds, Leeds, United Kingdom. 2. Institute of Membrane and Systems Biology, University of Leeds, Leeds, United Kingdom.
View other abstracts by:
Table 1. Effects of simulated application of 0.08 mM lidocaine. All values are percentages.
Where applicable, experiments conform with Society ethical requirements.