Background: Haematopoietic stem cell transplantation (HSCT) is a life-saving treatment for childhood cancers and other life-threatening immunological and haematological diseases. The first HSCT-survivors are now reaching middle age1, and with this, long-term effects of previous disease and HSCT, such as reduced muscle mass and strength2, are appearing. It remains unclear if these changes are due to an inactive lifestyle or are a consequence of cellular damage from the high-dose cytotoxic therapies used in HSCT. Concerns over early onset sarcopenia in this population underscore the need for effective interventions. This study aimed to investigate the cellular mechanisms behind reduced muscle function in HSCT-survivors and evaluate their muscle’s ability to respond to acute and long-term heavy resistance exercise training (RET).
Methods: Two prospective, controlled intervention studies were conducted, focusing on the effects of one session (1RET) or 36 sessions (36RET) of RET. 36RET was pre-registered (ClinicalTrials: NCT04922970) with quadriceps cross-sectional area (CSA) as the primary outcome. Following ethical approval, 12 female (27±5 year, 23±4 BMI) and 6 male (31±7 year, 21±3 BMI) HSCT-survivors and 18 female (29±7 year, 23±4 BMI) and 10 male (30±8 year, 24±2 BMI) age-matched controls were recruited. 1RET included 7 HSCT-survivors and 11 controls, and 36RET included 11 HSCT-survivors and 17 controls. In 1RET, participants performed one bout of RET with one leg and came in for evaluation 7 days after. In 36RET, participants performed 12 weeks (36 sessions) of RET. Leg extension maximal voluntary contraction (MVC), thigh magnetic resonance imaging, Dual-Energy X-ray Absorptiometry, and muscle biopsies were conducted. Muscle biopsies were analysed for myofibre denervation and size, and content of satellite cells (MuSC), myonuclei and fibroblasts. Parametric (mean±SD) or nonparametric statistical analyses were used based on data distribution.
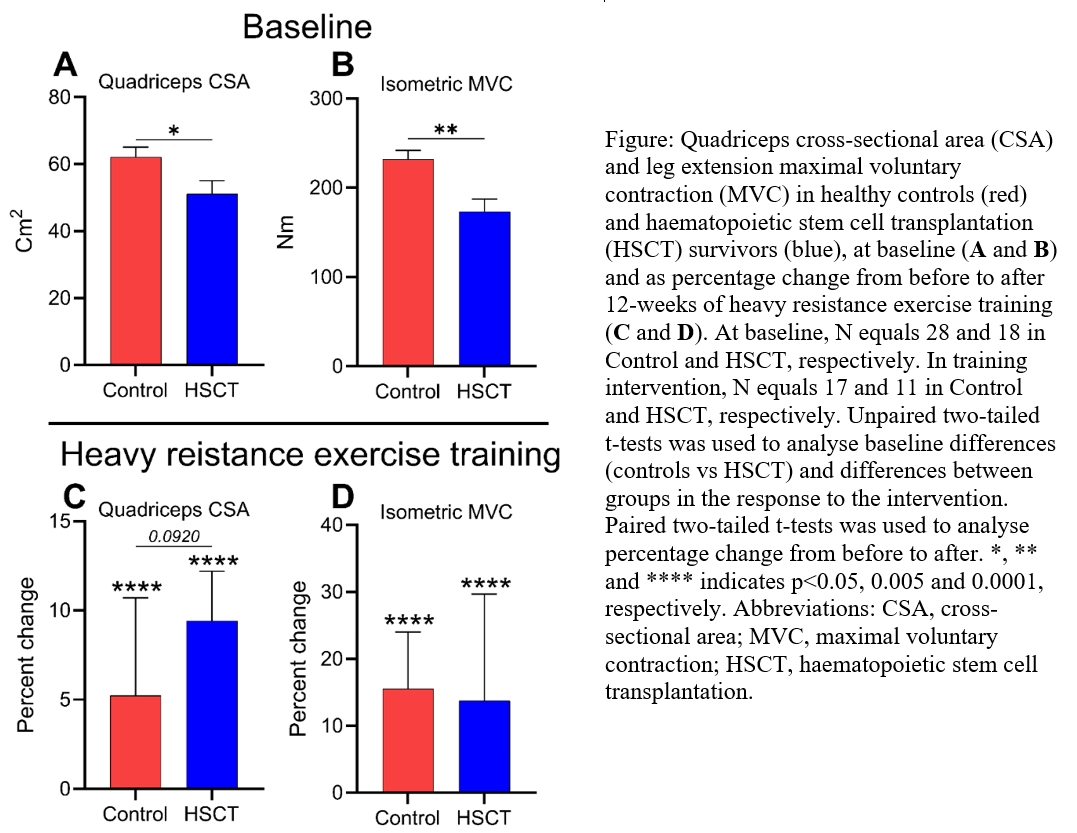
Results: At baseline, HSCT-survivors had 19% smaller quadriceps CSA (fig.1.A, p<0.05), 17% less leg lean mass (LLM) (p<0.0.05), and 29% lower MVC (fig.1.B, p<0.005), compared to controls. In the muscle biopsies, similar levels of MuSC, myonuclei and fibroblasts were observed in HSCT-survivors and controls. The CSA of type II myofibres was 30% smaller in HSCT-survivors, albeit only in males (p<0.05). Myofibre type grouping (p<0.05) and fibre denervation (tendency, p=0.055) was more pronounced in HSCT-survivors. The 1RET was strenuous (rating of perceived exertion 7±1 (scale to 10) and led to a 21±9% reduction MVC post exercise (p<0.0001). No changes were observed in numbers of MuSC, myonuclei and fibroblasts following 1RET. In 36RET, similar increments for HSCT-survivors and controls were observed in quadriceps CSA (fig.1.C, 4.9±1.4 and 3.0±3.2 cm, p<0.0001), LLM (441±295 and 721±1266 g, p<0.05), MVC (fig.1.D, 23±33 and 35±18 Nm, p<0.0001) and type II myofibre CSA (614±776 and 189±747 μm2, p<0.05). No changes were observed in numbers of MuSC, myonuclei and fibroblasts following 36RET.
Conclusion: This study identifies specific physiological characteristics making up the inferior neuromuscular profile of HSCT-survivors. With 12-weeks of RET, a similar magnitude of improvement was observed in HSCT-survivors and controls, demonstrating a preserved capacity for neuromuscular adaptation in HSCT-survivors. These findings highlight the potential of RET to mitigate the long-term consequences of paediatric HSCT.