Introduction
More than 64 million people suffered from heart failure worldwide in 2017, and this number is expected to be growing (1). Originally, sodium-glucose cotransporter-2 (SGLT2) inhibitors were used to treat type 2 diabetes, but several clinical studies have demonstrated their significant beneficial effects in patients with heart failure independent of their diabetic status (2). The underlying mechanisms are unknown, but intensively investigated. A recent study proposes that a part of the cardioprotective mechanism is a result of SGLT2 inhibition-related improvements in metabolic communication reflecting in the kidney (3). However, heart morphology and function were not investigated. Nevertheless, changes in cardiac metabolism are suggested to promote heart failure development, including left ventricular hypertrophy (4).
We hypothesized that SGLT2 inhibitors may reduce severity of heart failure by preventing cardiac remodeling due to an improved cardiometabolic state.
Methods
33 Bl57c6j male mice were randomly divided into the following 5 subgroups; I) mice on a normal diet, II) vehicle-treated mice on High Fat Diet (HFD); III) vehicle treated mice on HFD receiving N-nitro-1-arginine methyl ester (L-NAME, 600 mg/kg/day) in drinking water; IV) SGLT2 inhibitor-treated (dapagliflozin; 10 mg/kg diet (DAPA)) mice on HFD; and V) SGLT2 inhibitor-treated mice on HFD and L-NAME with all interventions lasting for 6-8 weeks. This combination of HFD and L-NAME was used to induce heart failure with preserved ejection fraction (5).
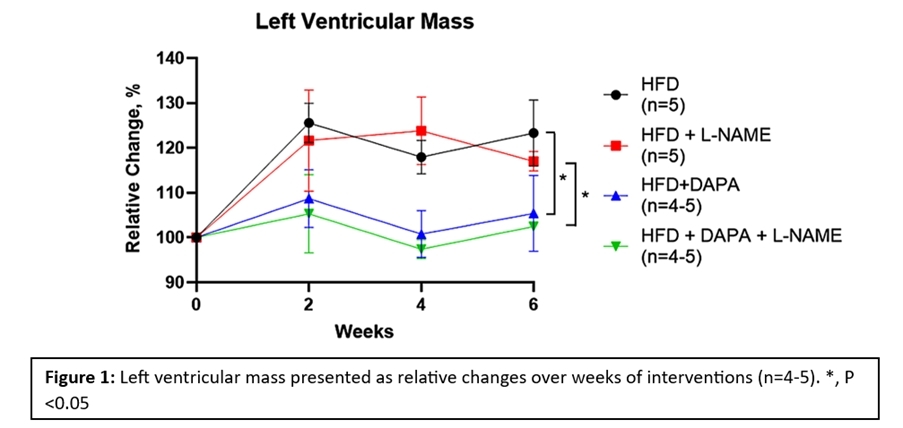
Blood pressure measurements and echocardiography were conducted before intervention and every 2nd week during the intervention period.
The protocol was conducted in accordance with the animal experiment permissions from the Danish Ministry of Food, Agriculture and Fisheries.
Data were analyzed using mixed-effects model followed by Tukey post-test for multiple comparison (GraphPad Prism 10.2.1). Data are presented as means ± standard errors of the means, P<0.05 is considered statistically significant.
Results
L-NAME increased mean arterial pressure in both groups receiving HFD and HFD+DAPA. Six weeks after intervention, mean arterial pressure was 91±4, 118±6, 89±2 and 122±6 mmHg (n=4-5, P=0.0004) in HFD, HFD+L-NAME, HFD+DAPA and HFD+DAPA+L-NAME, respectively. An increased heart rate by L-NAME was also observed in the group receiving HFD (588±9 BPM), but the effect was absent in the HFD+DAPA-group (545±16 BPM).
No difference was observed between the groups in stroke volume, ejection fraction, fractional shortening and cardiac output. However, the left ventricular mass was increased in the groups receiving HFD and HFD+L-NAME but this was prevented in both groups receiving DAPA (Figure 1).
Conclusion
Our results suggest that one of the mechanisms underlying SGLT2-inhibitor-related cardiac protection is its ability to reduce the development of left ventricular hypertrophy, which is a known part in the pathogenesis of heart failure.