Introduction:
The perception of skin wetness plays an important role in behavioural thermoregulation and thermal comfort (e.g. the onset of sweating). Whilst our understanding of the neurophysiology of skin wetness perception (WP) is expanding [1], research is lacking on how the biophysical status of the skin, such as its hydration levels, impacts local wetness sensitivity. Skin hydration levels can vary individually due to intrinsic (e.g. sex, age) and extrinsic factors (e.g. environment). Changes in the skin’ stratum corneum hydration could alter the skin’s properties leading to increased or decreased wetness sensitivity [2]. This study aimed to investigate the effect of skin hydration levels on local WP and its individual variability.
Method:
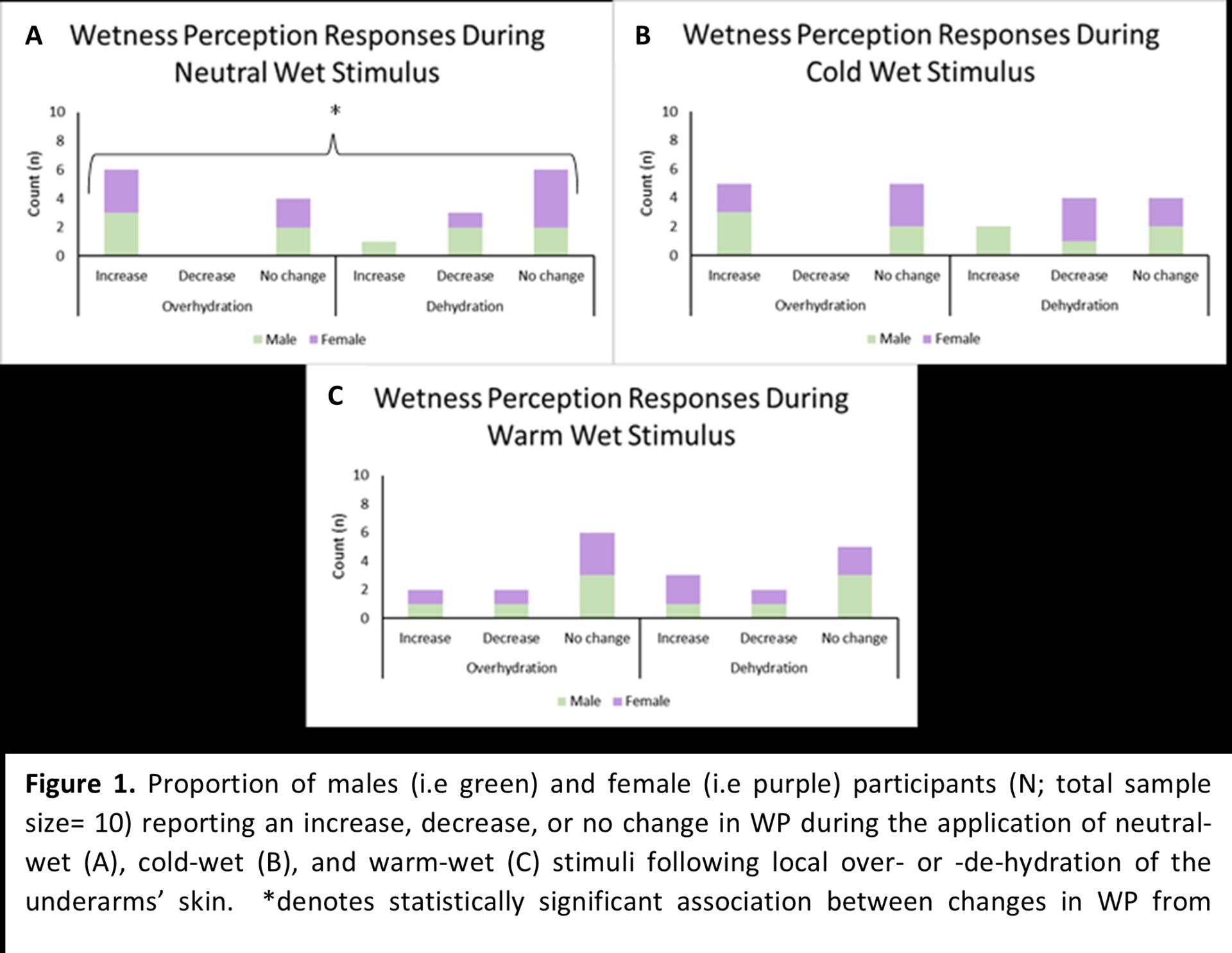
Ten male (n=5) and female (n=5) participants (28.8 ± 7.2y; 171.3 ± 9.5cm; 78.1 ± 18.2kg) took part in two separate experimental trials, during which they underwent a quantitative sensory test (QST) of WP at baseline and following localised overhydration [i.e. OVH; +22 ± 20% from baseline] or dehydration [i.e. DEH; -44 ± 20% from baseline] of the underarm’ skin. Participants reported on a 100-mm visual analogue scale the perceived magnitude of WP (anchor points: 0=dry; 100=completely wet) from the short-duration (i.e. 10s) static application of a cold-wet (i.e. 5°C below local skin temperature), neutral-wet (i.e. equal to local skin temperature) and warm-wet (i.e. 5°C above local skin temperature). Before the QST(s), local tactile sensitivity, skin temperature, stratum corneum hydration, and skin surface roughness were measured. Individual participants' perceptual responses to each temperature stimuli were coded as either A) a change in WP (i.e. ≥10-mm difference in WP from baseline to post OVH or DEH); or B) no change (i.e. <10-mm difference). Pearson's chi-squared tests of independence were used to examine the association between changes in WP from baseline and skin hydration status (i.e. OVH or DEH) for each temperature stimulus.
Results:
We found a statistically significant association [X² (2)=6.9, p= 0.03] between skin hydration status and changes in WP during neutral-wet stimulation. Specifically, 60% of participants reported an increase in WP following OVH, whilst 30% reported a decrease following DEH (Fig. 1A). A similar trend was observed during cold-wet stimulation [X² (2)= 5.4, p= 0.07) whereby 50% of participants reported an increase in WP following OVH, whilst 40% reported a decrease following DEH (Fig. 1B). No significant association was found between changes in WP and skin hydration status during warm-wet stimulation (X² (2)= 0.3, p= 0.865)(Fig.1C). Differences in the changes in WP following manipulation in hydration status were not explained by sex (Fig. 1).
Conclusion:
The study found that skin hydration levels may influence WP, although this effect is dependent on stimulus temperature. Furthermore, hydration-dependent changes in WP were observed in ~50% of the sample only. The response to the change in skin hydration state may be divided into subgroups of responders and non-responders, with individual variability modifying the effect of skin hydration levels on WP to a larger extent than sex-related differences.