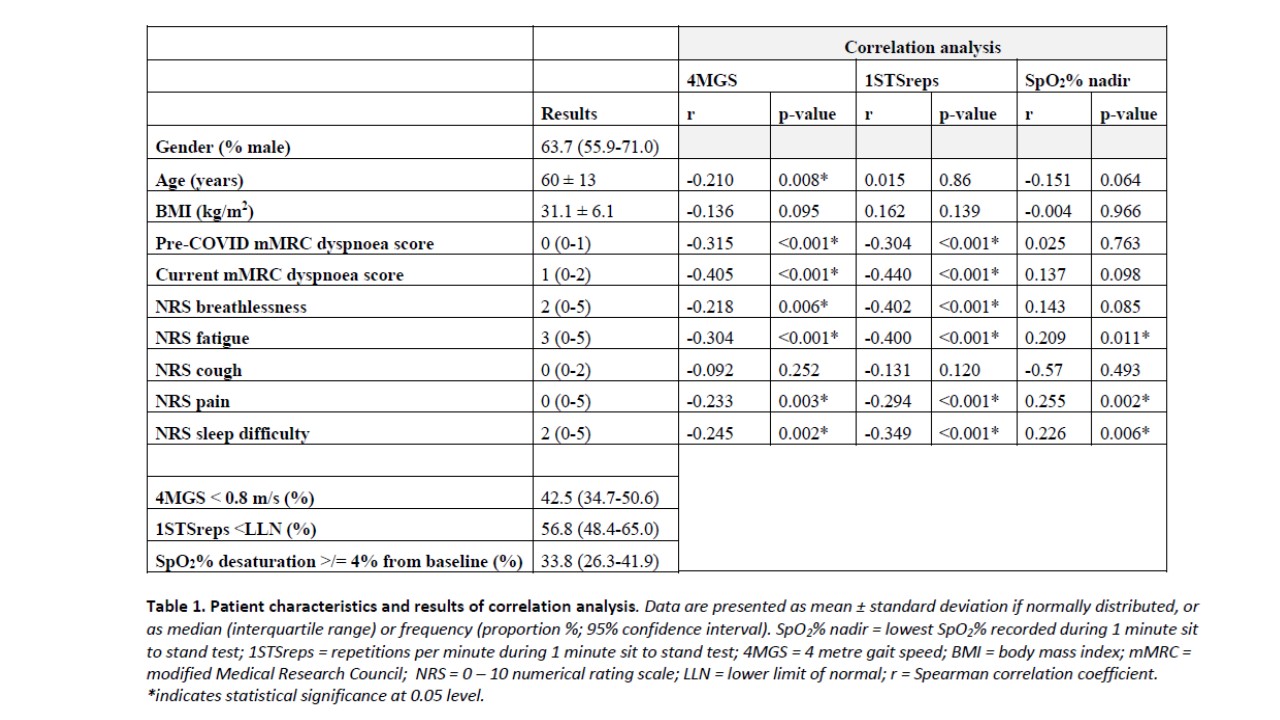
The COVID-19 pandemic has affected millions of people worldwide. Acute COVID-19 infection can cause persistent and burdensome symptoms, impacting physiological function and quality of life (D’Cruz et al., 2021). Ideally, holistic post-COVID assessment includes physiological tests, yet infection control policies favour remote assessment of symptoms where possible. The availability of tests involving aerosol generating procedures, such as spirometry, is restricted. This study aimed to investigate the relationship between patient-reported symptoms and physiological outcomes in survivors of severe COVID-19 pneumonia, to investigate the role of in-person physiological assessment. This was a prospective single-centre observational study in the outpatient department of an urban South London teaching hospital. Survivors of severe COVID-19 pneumonia were invited for face-to-face assessment at 4-6 weeks post hospital discharge. Relationships between subjective self-reported symptoms (outcome measures listed in Table 1), 4 metre gait speed (metres/second (4MGS)) (Hirabayashi et al., 2020), and 1 minute sit to stand (repetitions/min (1STSreps) and SpO2% desaturation) (Briand et al., 2018) were assessed using correlation and multiple regression analysis. 168 patients attended clinic between June and November 2020. Patient characteristics and results of correlation analysis are shown in Table 1. Age (Beta = -0.284, p<0.001) and current mMRC dyspnoea score (Beta= -0.352, p=0.001) were independent predictors of 4MGS (overall model fit R2=0.35, p<0.001). Body mass index was the only independent predictor of 1STSreps (Beta=0.214, p=0.007, overall model fit R2=0.33, p<0.001). NRS pain (Beta=0.298, p=0.004) and cough (Beta=-0.179, p=0.041) were the only independent predictors of SpO2% nadir during 1STS (overall model fit R2=0.13, p=0.039). Respiratory symptoms were not strong predictors of 4MGS and 1STS performance, emphasising the importance of objective physiological tests in post-COVID assessments. The challenge of providing holistic care to survivors of COVID-19 has highlighted the importance of clinical respiratory physiology to the multidisciplinary team.
Future Physiology 2021 (Virutal) (2021) Proc Physiol Soc 47, OC12
Oral Communications: Understanding the role of objective physiological tests in assessment of survivors of severe COVID-19 pneumonia
Sneha Mehrotra1, Parisa Zamani1, Rebecca F. D'Cruz1, Sheron Mathew2, Alice Byrne2, Mutahhara Choudhury2, Tracey Fleming2, Sam Norton3, Surinder Birring1, 2, Amit Patel1, 2, Irem Patel1, 2, Felicity Perrin2, Michael Waller1, 2, Caroline J. Jolley1, 2
1 Centre for Human and Applied Physiological Sciences, King's College London, King’s Health Partners, London, United Kingdom 2 Department of Respiratory Medicine, King's College Hospital NHS Foundation Trust, London, United Kingdom 3 Centre for Rheumatic Diseases, King's College London, London, United Kingdom
View other abstracts by:
Where applicable, experiments conform with Society ethical requirements.