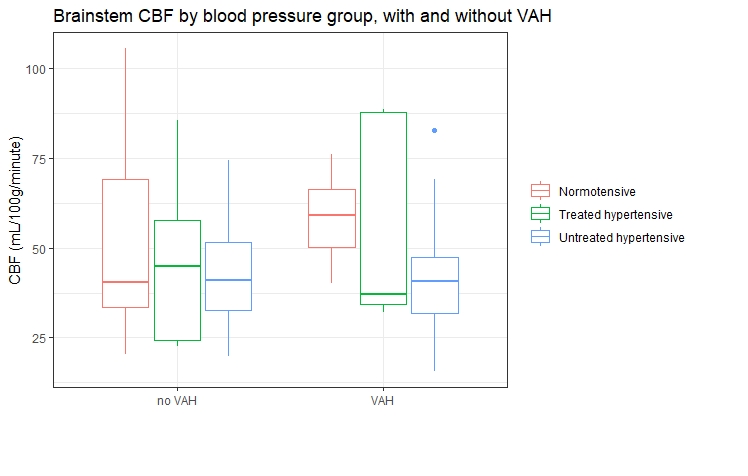
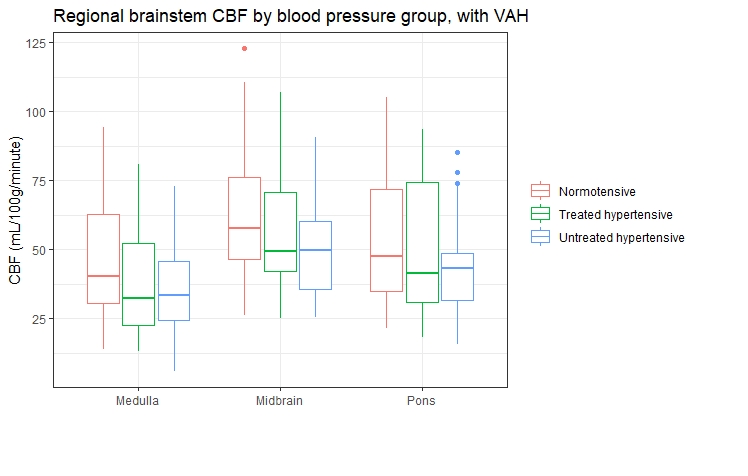
Hypertension is highly prevalent worldwide and is a risk factor for several diseases (1), but its aetiology is poorly understood (2). Cushing’s hypothesis proposes that hypertension is a compensatory mechanism that aims to correct cerebral blood flow (CBF) to regions of the brain responsible for cardiovascular autonomic control. These include the brainstem, within which the medulla plays an important role in autonomic regulation of the cardiovascular system. Our group previously showed an increased prevalence of vertebral artery hypoplasia (VAH) and a reduction in CBF in hypertensives compared to normotensives (3). A further analysis of this data was performed to investigate the impact of VAH on brainstem CBF, and whether this varies between normotensives, treated hypertensives and untreated hypertensives. Whole brain CBF maps acquired using arterial spin labelling magnetic resonance imaging (ASL MRI) were available for 80 participants (25 normotensives, 26 untreated hypertensives and 35 untreated hypertensives). Anatomical segmentation of a T1-weighted structural MRI scan was performed for each participant. The segmented regions of interest were applied to the CBF data to generate regional CBF values. A two-way ANCOVA was conducted to compare the effect of VAH (present or absent) and blood pressure (normotensive, treated hypertensive or untreated hypertensive) on brainstem CBF. The interaction between blood pressure and VAH was also modelled. Age, BMI and sex were included as covariates. To account for the positive skew of CBF data, values are reported as median [interquartile range]. There was no significant effect of VAH (F(1) = 0.07, p = 0.79, partial η2 = 0.001) , blood pressure (F(2) = 2.74, p = 0.07, partial η2 = 0.09) or the interaction between VAH and blood pressure (F(2) = 0.15, p = 0.87, partial η2 = 0.01) on CBF. However, there is a trend towards higher brainstem CBF in normotensives with VAH (normotensive CBF = 59 [16], untreated hypertensive CBF = 41 [16] and treated hypertensive CBF = 37 [54] mL/100g/minute) compared to those without VAH (normotensive CBF = 47 [35], untreated hypertensive CBF = 41 [19] and treated hypertensive CBF = 45 [34] mL/100g/minute). Subsequently a three-way ANCOVA was conducted to investigate the interaction between regional brainstem CBF (medulla, pons or midbrain), VAH and blood pressure. A similar trend was observed towards higher CBF in normotensives with VAH in all three brainstem regions including the medulla (medulla CBF with VAH 44 [23] (normotensive), 33 [23] (untreated), 25 [8] (treated) mL/100g/minute). There was no significant interaction between VAH, blood pressure and regional brainstem CBF (F(4) = 0.32, p = 0.86, partial η2 = 0.006). A trend towards a higher brainstem CBF in normotensives with VAH is unexpected and contrary to Cushing’s hypothesis. On the other hand, within the VAH group, a trend towards a lower regional brainstem CBF in hypertensives with VAH raises the possibility that VAH creates a fixed resistance to brainstem CBF in hypertensives. The cross-sectional nature of the data precludes any inferences about causation. An adequately powered longitudinal study is required to further explore the causative nature of these relationships.
Physiology 2021 (2021) Proc Physiol Soc 48, OC26
Oral Communications: Vertebral artery hypoplasia and brainstem blood flow in patients with hypertension
Bleddyn Woodward1, Esther Warnert2, Emma C. Hart3, Ian Driver1, Richard Wise1
1 Cardiff University, Cardiff, United Kingdom 2 Erasmus MC, Rotterdam, The Netherlands 3 Bristol University, Bristol, United Kingdom
View other abstracts by:
Where applicable, experiments conform with Society ethical requirements.