Jeanette M Bennett, University of North Carolina at Charlotte, USA
Danilo Bondi, University “G. d’Annunzio” of Chieti, Pescara, Italy
What do heart rate variability impairment, oral dysbiosis, and systemic inflammation have in common? They are all indicators of dis-stressed human physiology.
With the rise in non-communicable diseases and the wide variation in communicable illness severity (e.g., SARS-CoV-2), establishing biomarkers of human health is needed to aid healthcare professionals in identifying individuals at risk of morbidity and mortality.
We know that disrupted biological functioning can lead to adaptations, changing health and illness experiences.
Our recent webinar hosted by The Physiological Society called Summary Indexes of Health: Markers as Outcomes of Variability, Complexity, and Systemic Adaptations featured cutting-edge, original research that offers clues into the complex, interconnected networks of physiological functioning via biomarkers to examine health.
Heart rate variability as a dynamic hallmark of health
Within the framework of physiological variability, heart rate has been leading the way. As Dr Fred Shaffer pointed out, beyond heart rate alone, vagally-mediated heart rate variability (HRV) plays a vital role in regulating executive functions (such as working memory and cognitive flexibility), health, and performance.
Reduced vagally-mediated HRV is associated with disease and loss of physiological adaptation to external and internal stressors.
As a result, clinicians have been using HRV biofeedback to treat diverse disorders (e.g., asthma and depression) and enhance performance in a variety of contexts (e.g., sports) (1).
Successful HRV biofeedback training can increase some indexes of vagal tone at normal breathing pace (12-14 breaths/minute [bpm]) over weeks to months of practice.
For healthy individuals, we should only expect to see elevated low frequency (LF) power during slow-paced breathing (6-8 bpm). In fact, high LF power at normal breathing pace may signal that the vagal brake is malfunctioning.
The oral cavity is not a closed niche
Among the body districts that are linked to distant pathophysiological processes, the oral cavity represents a very interesting environment.
As suggested by Peres and colleagues (2019), “Oral health is an integral element of overall health and wellbeing… Despite being largely preventable, oral diseases are highly prevalent conditions” (2).
Dr Pamela Pignatelli reminded us that over 50% of the European population suffer from some form of periodontitis and over 10% have severe disease, with prevalence increasing with age (3).
In periodontal diseases, polymicrobial communities stimulate a dysfunctional and deleterious response of the host, through a mechanism called “polymicrobial synergy and dysbiosis”.
The chemical communication between oral microbes can increase the pathogenicity of key species, resulting in proinflammatory changes or dysbiosis within the oral cavity, like as periodontal disease.
Indeed, polymicrobial infections that involve a group of interacting bacteria species synergistically producing a pathogenic effect are more complex to treat than a single-species infection.
Systemic conditions can manifest in the oral cavity, and periodontal disease is comorbid with systemic non-communicable diseases such as diabetes, colon cancer, cardiovascular and neurodegenerative diseases (3).
Tackling the environmental-to-biological transition through the approach of systemic inflammation
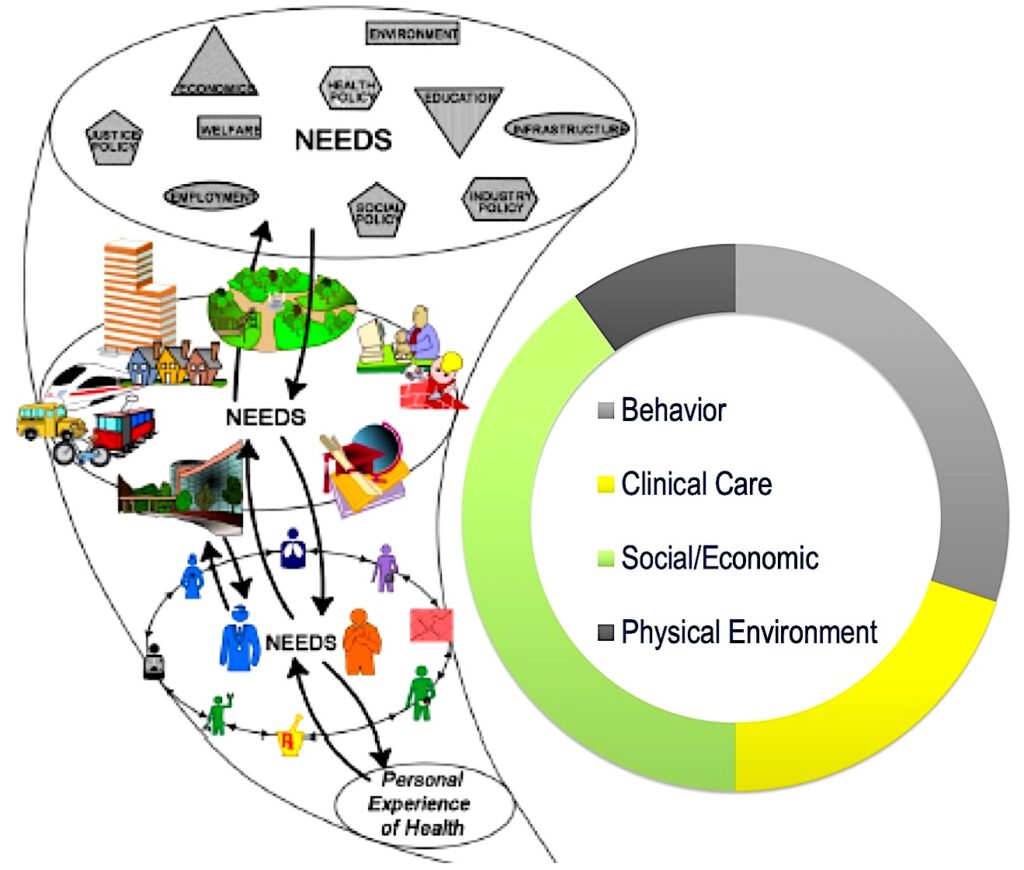
Extrinsic factors exert their beneficial and deleterious effects acting through physiological and pathophysiological processes, how the outside world gets under the skin. Emerging and resurging diseases, as well as the broad topics of health and diseases, recently have been addressed by the “one health” approach (4).
Within this bio-social framework, Dr Raphaële Castagné discussed the effects of adversity (e.g., lower socioeconomic positions, adverse childhood experiences) across the lifespan utilizing the theoretical framework of bio-social model (5).
Allostatic load, as the summation of four physiological systems (neuroendocrine, cardiopulmonary, metabolic, and immune), predicted subsequent all-cause mortality better than any of its individual parts.
However, immune-mediators as indexed by C-reactive protein (CRP) and fibrinogen, and cardiopulmonary measures, including heart rate and peak flow independently, appeared to predict a nearly similar level of the cumulative probability of death as the total allostatic load measure.
It is too early to tell if these four physiological indicators are universally just as predictive of mortality as the more global allostatic load or was this finding unique to the sample utilized in the study (5).
Conclusions
Internal physiological functioning and the external context converge on the human body in daily living.
In a dis-stressed body, dysregulation can be indexed by specific indicators, but all can be linked to impaired inter-organ interconnections, emergent non-resolving inflammation, and poorly functioning immune and/or neuroendocrine systems.
Rebalancing activity of autonomic nervous system at rest toward greater parasympathetic activity might be the biggest takeaway for treating stress-related effects on health.
HRV biofeedback could be a useful tool moving forward. An anti-inflammatory lifestyle should allow individuals to develop or maintain optimal health trajectories across lifespan (6).
This webinar was part of the broader series called The Emergence of Health: Navigating through Mechanisms, Drivers, Hallmarks and Analyses”. For more information on The Physiological Society’s upcoming events, click here.
References
- Shaffer, F., & Meehan, Z. M. (2020). A Practical Guide to Resonance Frequency Assessment for Heart Rate Variability Biofeedback. Frontiers in Neuroscience, 14, 570400. https://doi.org/10.3389/fnins.2020.570400
- Peres, M. A., Macpherson, L. M. D., Weyant, R. J., Daly, B., Venturelli, R., Mathur, M. R., Listl, S., Celeste, R. K., Guarnizo-Herreño, C. C., Kearns, C., Benzian, H., Allison, P., & Watt, R. G. (2019). Oral diseases: A global public health challenge. The Lancet, 394(10194), 249–260. https://doi.org/10.1016/S0140-6736(19)31146-8
- Pignatelli, P., Iezzi, L., Pennese, M., Raimondi, P., Cichella, A., Bondi, D., Grande, R., Cotellese, R., Di Bartolomeo, N., Innocenti, P., Piattelli, A., & Curia, M. C. (2021). The Potential of Colonic Tumor Tissue Fusobacterium nucleatum to Predict Staging and Its Interplay with Oral Abundance in Colon Cancer Patients. Cancers, 13(5), 1032. https://doi.org/10.3390/cancers13051032
- Mackenzie, J. S., & Jeggo, M. (2019). The One Health Approach—Why Is It So Important? Tropical Medicine and Infectious Disease, 4(2), 88. https://doi.org/10.3390/tropicalmed4020088
- Castagné R et al. (2018). Allostatic load and subsequent all-cause mortality: Which biological markers drive the relationship? Findings from a UK birth cohort. European Journal of Epidemiology, 33(5), 441–458. https://doi.org/10.1007/s10654-018-0364-1
- Bennett JM et al. (2018). Inflammation-Nature’s Way to Efficiently Respond to All Types of Challenges: Implications for Understanding and Managing “the Epidemic” of Chronic Diseases. Frontiers in Medicine, 5, 316. https://doi.org/10.3389/fmed.2018.00316
- Refinetti, R. (2008). Biological Rhythms. In B. Fath (Ed.), Encyclopedia of Ecology (Second Edition) (pp. 163–169). Elsevier. https://doi.org/10.1016/B978-0-444-63768-0.00007-X
