By Dr Jessica S. Smyth, Postdoctoral Researcher in the Gastroenterology Research Group, The Royal College of Surgeons in Ireland
“There are in fact two things, science and opinion; the former begets knowledge, the latter ignorance”. Being a scientist, this quote is one of my favourites. It is accredited to the ancient Greek physician Hippocrates, the universally considered “Father of Medicine”, long revered for his contributions to advancing the study of clinical medicine and for allegedly composing a code of principles on the ideals and ethical standards of the physician.
Another statement attributed to Hippocrates is that “All disease begins in the gut”, which may initially seem like an exaggerated claim. However, scientific research has increasingly supported the idea that the gut plays a fundamental role in our overall health and well-being and that the impact of gut health on disease development is profound.
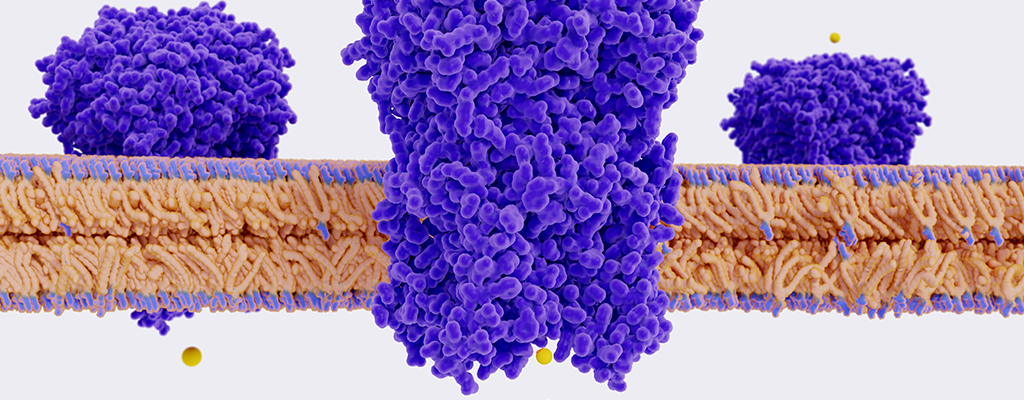
The main player in the maintenance of a healthy gut is the intestinal epithelium, a single layer of cells that line the small and large intestines. These cells transport fluid, electrolytes, and nutrients to and from the intestinal lumen and form a protective barrier that restricts the entry of harmful pathogens.
Dysregulation of these processes is known to contribute to the development of intestinal diseases such as inflammatory bowel disease and colorectal cancer, and has also been linked to other conditions such as cardiovascular disease, obesity and diabetes, and mental health disorders, such as anxiety and depression1-3.
For the last five and a half years, as a budding gastrointestinal physiologist in the Gastroenterology Research Group in RCSI, headed by Dr Stephen Keely, I have been researching the effects of bile acids on the intestinal epithelium. These steroid molecules, classically known for their role in fat digestion, are now also recognised as important signalling hormones that influence many aspects of intestinal epithelial function4.
The first identified bile acid receptor, farnesoid X receptor (FXR), is now appreciated not only as a master regulator of bile acid homeostasis but also as a transcription factor with a wide range of biological effects. Since its discovery, our understanding of FXR’s role in preventing the onset and progression of intestinal disease has grown exponentially and its protective effects in conditions such as chronic diarrhoea, inflammatory bowel disease, and colorectal cancer are clear5-11.
This makes FXR an attractive target for the development of new therapeutics. However, despite the growing evidence, there are still no FXR-targeted therapeutics approved for use in these conditions.
Our research in the lab aims to change this with one aspect of our work focusing on using nutraceuticals to target FXR. A nutraceutical is defined as ‘any substance that is a food or part of a food and provides medical or health benefits, including the prevention and treatment of disease’12.
This isn’t a new concept. In fact, to quote him a third time, the wise Hippocrates once said “Let food be thy medicine and medicine be thy food”. Even in the 5th century BCE the connection between our diet and our overall health was well appreciated and it was believed that the foods we consume have the power to prevent and treat illness.
The list of known nutraceuticals is ever-expanding but common examples in use today include omega-3 fatty acids, known for their importance in maintaining a healthy heart and brain; folate, a B vitamin that is crucial during early pregnancy to prevent brain and spinal cord defects; and curcumin, a bright yellow compound found in turmeric that is appreciated for its powerful antioxidant and anti-inflammatory properties13-16.
Recent work from our lab has shown that pentacyclic triterpenes, a class of plant-derived compounds found in plant leaves, stem bark, and fruit peel, can increase the levels of FXR found in colonic epithelial cells17. This in turn allows for further activation of the receptor, which could be translated into greater therapeutic benefits for treating intestinal disease.
I’m looking forward to speaking about this topic in greater detail and about the impact of targeting FXR on chloride secretion and diarrhoeal disease at Membrane Transport 2023 which takes place on the 24 and 25 August at the University of St Andrews, Scotland. Having attended many meetings organised by the Epithelia and Membrane Transport group throughout my training, these events give early career researchers like me an excellent and exciting opportunity to present our work and network with leading physiologists from around the globe!
Register now for our event Membrane Transport 2023. Secure your place for our two-day meeting from 24-25 August at the University of St Andrews to explore the latest research in epithelial transport physiology, ion channels and the latest emerging techniques in the field.
References
- Lewis CV, Taylor WR. Intestinal barrier dysfunction as a therapeutic target for cardiovascular disease. Am J Physiol Heart Circ Physiol. 2020;319(6):H1227-h1233.
- Riedel S, Pheiffer C, Johnson R, Louw J, Muller CJF. Intestinal Barrier Function and Immune Homeostasis Are Missing Links in Obesity and Type 2 Diabetes Development. Front Endocrinol (Lausanne). 2021;12:833544.
- Kelly JR, Kennedy PJ, Cryan JF, Dinan TG, Clarke G, Hyland NP. Breaking down the barriers: the gut microbiome, intestinal permeability and stress-related psychiatric disorders. Front Cell Neurosci. 2015;9:392.
- Hegyi P, Maléth J, Walters JR, Hofmann AF, Keely SJ. Guts and Gall: Bile Acids in Regulation of Intestinal Epithelial Function in Health and Disease. Physiological Reviews. 2018;98(4):1983-2023.
- Mroz MS, Keating N, Ward JB, et al. Farnesoid X receptor agonists attenuate colonic epithelial secretory function and prevent experimental diarrhoea in vivo. Gut. 2014;63(5):808-817.
- Walters JR, Johnston IM, Nolan JD, Vassie C, Pruzanski ME, Shapiro DA. The response of patients with bile acid diarrhoea to the farnesoid X receptor agonist obeticholic acid. Aliment Pharmacol Ther. 2015;41(1):54-64.
- Gadaleta RM, van Erpecum KJ, Oldenburg B, et al. Farnesoid X receptor activation inhibits inflammation and preserves the intestinal barrier in inflammatory bowel disease. Gut. 2011;60(4):463-472.
- Modica S, Gofflot F, Murzilli S, et al. The intestinal nuclear receptor signature with epithelial slocalisation patterns and expression modulation in tumors. Gastroenterology. 2010;138(2):636-648, 648.e631-612.
- Torres J, Bao X, Iuga AC, et al. Farnesoid X receptor expression is decreased in colonic mucosa of patients with primary sclerosing cholangitis and colitis-associated neoplasia. Inflamm Bowel Dis. 2013;19(2):275-282.
- Bailey AM, Zhan L, Maru D, et al. FXR silencing in human colon cancer by DNA methylation and KRAS signaling. Am J Physiol Gastrointest Liver Physiol. 2014;306(1):G48-58.
- Lax S, Schauer G, Prein K, et al. Expression of the nuclear bile acid receptor/farnesoid X receptor is reduced in human colon carcinoma compared to nonneoplastic mucosa independent from site and may be associated with adverse prognosis. Int J Cancer. 2012;130(10):2232-2239.
- DeFelice SL. The nutraceutical revolution: its impact on food industry R&D. Trends in Food Science & Technology. 1995;6(2):59-61.
- Shen S, Gong C, Jin K, Zhou L, Xiao Y, Ma L. Omega-3 Fatty Acid Supplementation and Coronary Heart Disease Risks: A Meta-Analysis of Randomized Controlled Clinical Trials. Front Nutr. 2022;9:809311.
- Dighriri IM, Alsubaie AM, Hakami FM, et al. Effects of Omega-3 Polyunsaturated Fatty Acids on Brain Functions: A Systematic Review. Cureus. 2022;14(10):e30091.
- Greenberg JA, Bell SJ, Guan Y, Yu YH. Folic Acid supplementation and pregnancy: more than just neural tube defect prevention. Rev Obstet Gynecol. 2011;4(2):52-59.
- Kunnumakkara AB, Bordoloi D, Padmavathi G, et al. Curcumin, the golden nutraceutical: multitargeting for multiple chronic diseases. Br J Pharmacol. 2017;174(11):1325-1348.
- Fallon CM, Smyth JS, Quach A, et al. Pentacyclic triterpenes modulate farnesoid X receptor expression in colonic epithelial cells: Implications for colonic secretory function. J Biol Chem. 2022;298(11):102569.