By Georgina Ellison-Hughes, Professor of Regenerative Muscle Physiology, King’s College London
With the COVID-19 pandemic claiming tens of thousands of lives to date and a vaccine likely to be at least 12 months away, researchers are turning to other strategies for treating patients. A stem cell treatment has shown positive results in a clinical trial of seven patients with pneumonia due to COVID-19 in China.
COVID-19 attacks the lungs and airways, causing the immune system to leap into action.
In serious cases of COVID-19, the immune system can overreact and cause what’s called a cytokine storm. Think of cytokines like emergency response coordinators, telling ambulances where to go to deal with problems. However, sometimes the body’s response to infection can go into overdrive. That’s like lots of coordinators telling lots of ambulances to go to one emergency.
Cytokines normally recruit immune cells to fight the infection, but too many of them can cause a range of problems. Inviting too many immune cells around to the site of infection can cause the area to swell, which is called edema. Cytokines can also cause problems with gas exchange; this happens in the branching structure of our lungs, where oxygen flows into the blood and carbon dioxide flows out. Finally, they can cause acute respiratory distress syndrome (where the lungs fail to provide our bodies with enough oxygen), damage to our heart tissue, and a secondary infection. Any of these complications can lead to death.
Therefore avoiding, preventing or attenuating the cytokine storm may be key for the treatment of COVID-19 infected patients.
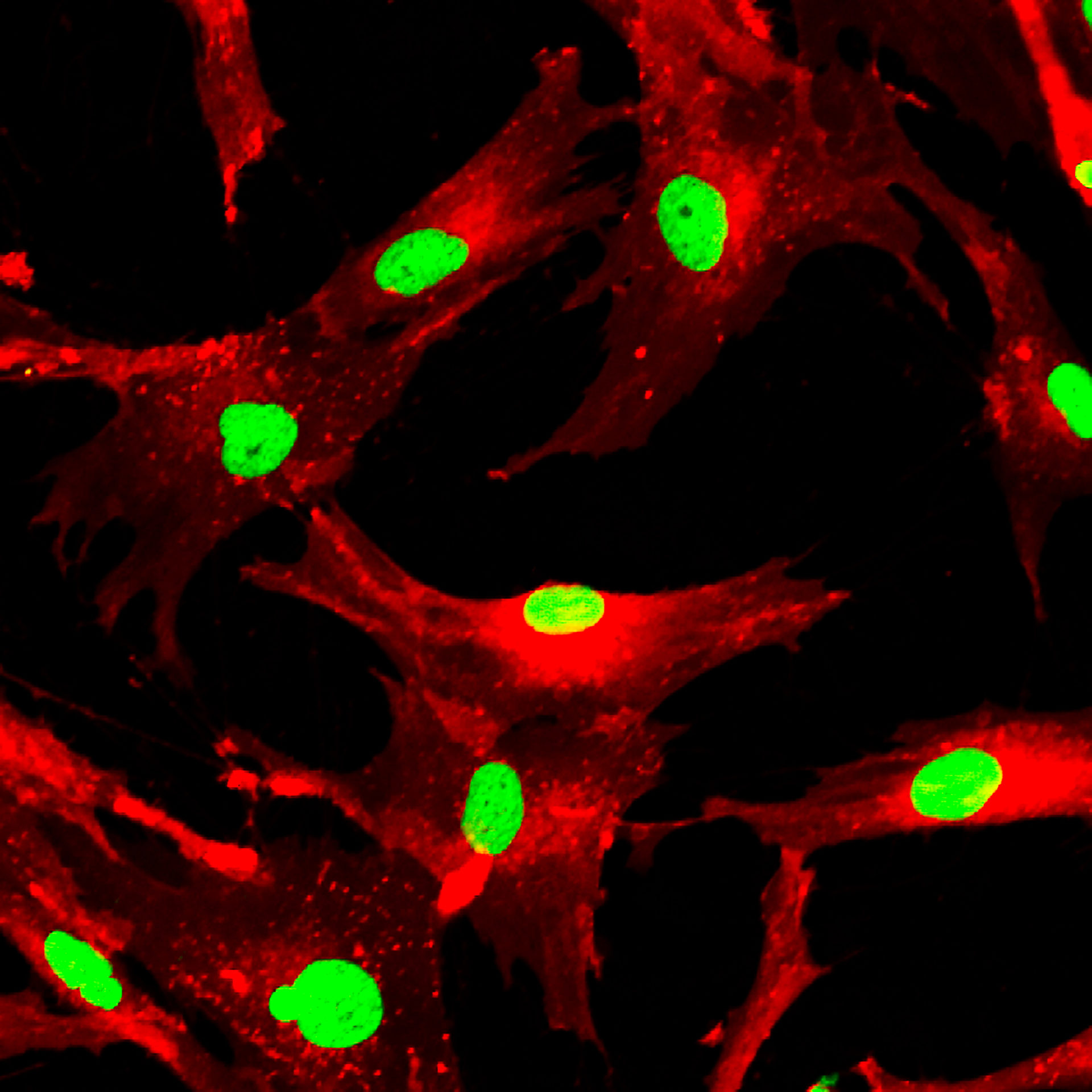
A specific type of stem cell, called mesenchymal stem cells or MSCs, are special cells found in our bone marrow. They’re special because they can transform into different types of cells such as cartilage, bone, tendons, muscle, and skin. They might be particularly useful for those suffering from COVID-19 because they can modify our body’s immune response, potentially preventing that dangerous cytokine storm.
Together with my colleagues, we are working on a clinical trial on patients with pneumonia due to COVID-19 in China. We injected one million MSCs per kg of body weight into the bloodstream of seven patients and observed them over 14 days.
Before the transplant, all the patients had COVID-19 pneumonia, with symptoms of high fever, weakness, shortness of breath and low oxygen levels in their blood. Results showed that all symptoms had disappeared by 2-4 days after the transplantation. This was not the case in the three placebo control patients. Among the MSC treated patients, one severe and two common patients were able to make a recovery and were able to be discharged 10 days after treatment.
This quick recovery could be a game-changer for wards that are currently overwhelmed by patients who spend much longer recovering. By testing this therapy in more patients, we hope to get a better idea of the patients who respond most robustly, whether that be more severe cases, specific age groups, or a certain sex.
Our team is now part of a global study with clinical trials happening in London to see whether they can replicate the results in hundreds more patients with severe COVID-19 infection.