Jorge Lopez-Tello, @JLopTello, University of Cambridge, UK
Jorge Lopez-Tello presented this work as part of our “Physiology of Obesity: From Mechanisms to Medicine” early career series. Sign up for upcoming webinars here: https://www.physoc.org/events/
In mammals, pregnancy is a unique physiological state in which the mother must adapt her metabolism to cover her own metabolic needs whilst promoting the growth her baby.
Changes in the metabolism of the mother are dynamic. In fact, changes in the body systems of the mother occur throughout gestation based on the requirements of her developing offspring.
During early pregnancy, when the requirements for growth of the offspring are relatively low, the mother expands her tissues, such as the liver, adipose, pancreas and kidneys. In contrast, in late gestation, the mother becomes insulin resistant and fat stores reduce to increase sugar and fats available for fetal growth (1).
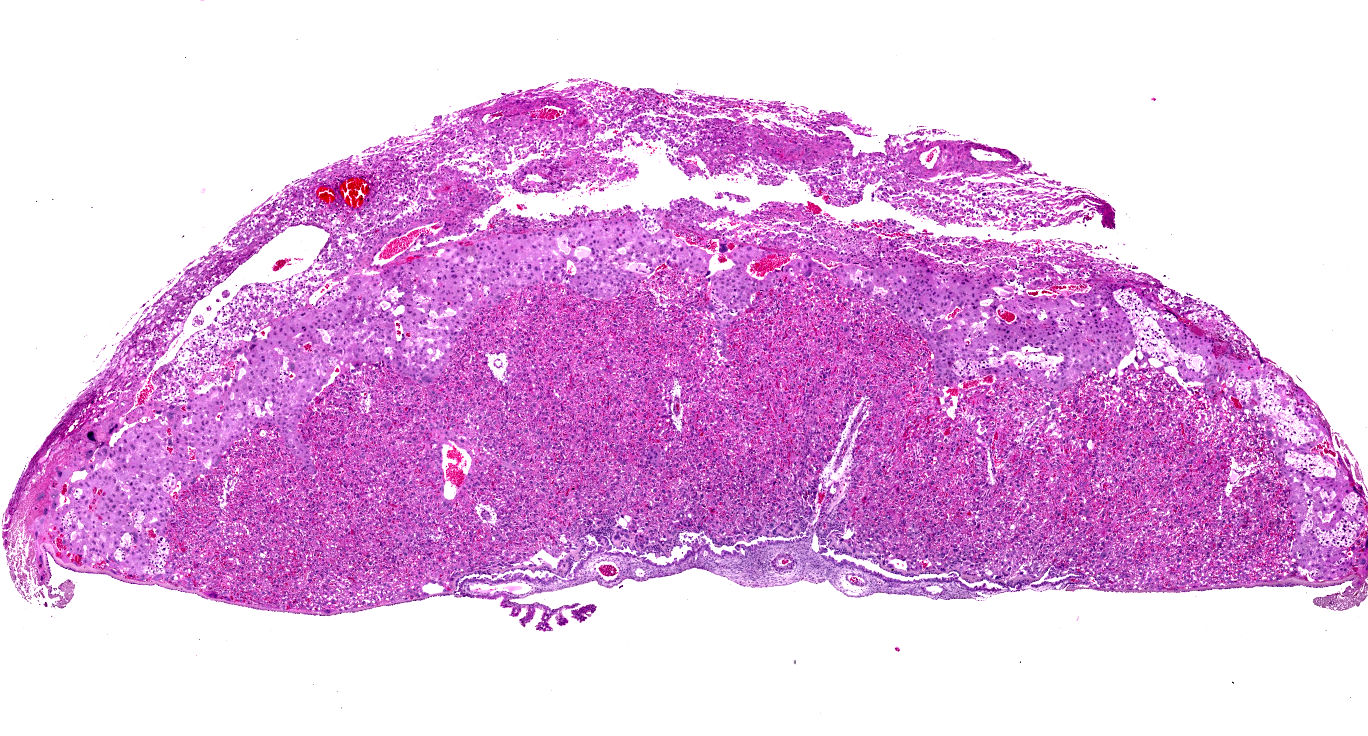
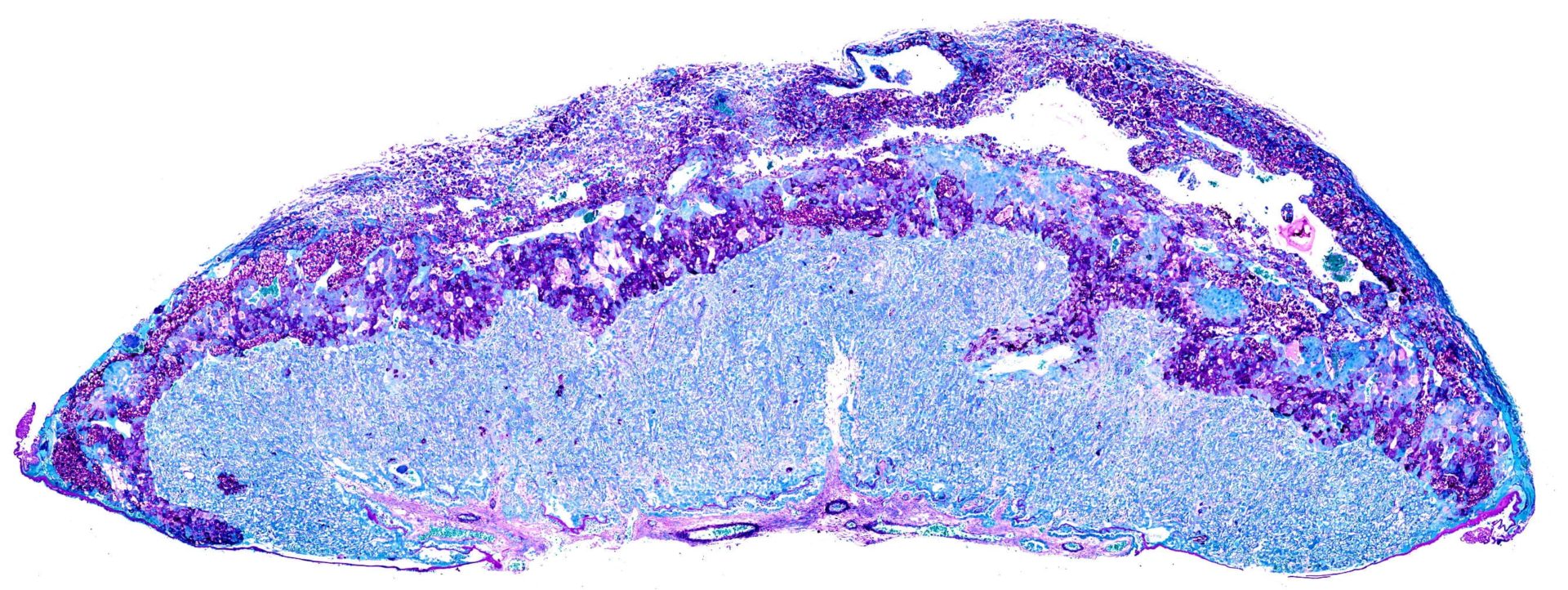
The metabolism of the mother during gestation is thought to be regulated, in part, by the placenta. Aside from transporting nutrients and gases between the mother and the fetus, the placenta acts as a powerful endocrine organ (2).
Hormones produced by the placenta, including placental lactogen, prolactin, progesterone and estrogen, influence maternal metabolism by modulating insulin secretion by the pancreas and the response of tissues such as the liver, skeletal muscle and adipose tissue to the action of insulin (3-7).
Situations in which the placenta does not function correctly (also called placental insufficiency) can lead to pregnancy complications, such as gestational diabetes (GDM).
This incredibly prevalent condition, which occurs in about one in every sex pregnancies, is defined by poor blood sugar control in the mother that is first recognised during pregnancy (8).
This is worrying as GDM is associated with other pregnancy complications such as preeclampsia (characterised by high blood pressure) and abnormal birthweight. Furthermore, GDM can predispose the mother and her child to developing Type 2 diabetes in later life (9,10).
During my postdoctoral training in Amanda Sferruzzi-Perri’s laboratory at the Centre for Trophoblast Research (University of Cambridge), supported by a Sir Henry Wellcome Fellowship, I will be studying a mouse model that has altered placental endocrine function to find out if placental hormones drive changes in the metabolism that lead to GDM in the mother.
Furthermore, I hope to identify which hormones are involved in this disease process and examine how they induce changes in the mother and her offspring that increase their susceptibility to developing metabolic diseases later in life.
A better understanding of the mechanisms controlling maternal metabolism during pregnancy will help us develop diagnostic, preventive and therapeutic strategies against the development of GDM and its associated long-term consequences in the mother and her offspring.
References
- N. Sferruzzi-Perri, J. Lopez-Tello, T. Napso, H.E.J. Yong, Exploring the causes and consequences of maternal metabolic maladaptations during pregnancy: Lessons from animal models, Placenta. (2020). https://doi.org/10.1016/j.placenta.2020.01.015.
- Napso, H. Yong, J. Lopez-Tello, A.N. Sferruzzi-Perri, The role of placental hormones in mediating maternal adaptations to support pregnancy and lactation, Front. Physiol. 9 (2018). https://doi.org/10.3389/fphys.2018.01091.
- A. Barbour, J. Shao, L. Qiao, L.K. Pulawa, D.R. Jensen, A. Bartke, M. Garrity, B. Draznin, J.E. Friedman, Human placental growth hormone causes severe insulin resistance in transgenic mice, Am. J. Obstet. Gynecol. 186 (2002) 512–517.
- C. Brelje, L.E. Stout, N.V. Bhagroo, R.L. Sorenson, Distinctive roles for prolactin and growth hormone in the activation of signal transducer and activator of transcription 5 in pancreatic islets of langerhans, Endocrinology. 145 (2004) 4162–4175. https://doi.org/10.1210/en.2004-0201.
- Huang, F. Snider, J.C. Cross, Prolactin receptor is required for normal glucose homeostasis and modulation of beta-cell mass during pregnancy, Endocrinology. 150 (2009) 1618–1626. https://doi.org/10.1210/en.2008-1003.
- Vejrazkova, J. Vcelak, M. Vankova, P. Lukasova, O. Bradnova, T. Halkova, R. Kancheva, B. Bendlova, Steroids and insulin resistance in pregnancy, J. Steroid Biochem. Mol. Biol. 139 (2014) 122–129. https://doi.org/10.1016/j.jsbmb.2012.11.007.
- Liao, M.H. Vickers, J.L. Stanley, A.P. Ponnampalam, P.N. Baker, J.K. Perry, The Placental Variant of Human Growth Hormone Reduces Maternal Insulin Sensitivity in a Dose-Dependent Manner in C57BL/6J Mice, Endocrinology. 157 (2016) 1175–1186. https://doi.org/10.1210/en.2015-1718.
- IDF Diabetes Atlas, (n.d.). https://www.idf.org/e-library/epidemiology-research/diabetes-atlas (accessed December 7, 2019).
- Bellamy, J.-P. Casas, A.D. Hingorani, D. Williams, Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis, Lancet. 373 (2009) 1773–1779. https://doi.org/10.1016/S0140-6736(09)60731-5.
- J. Monteiro, J.E. Norman, G.E. Rice, S.E. Illanes, Fetal programming and gestational diabetes mellitus, Placenta. 48 Suppl 1 (2016) S54–S60. https://doi.org/10.1016/j.placenta.2015.11.015.
