Physiology News Magazine
Air pollution and me
What do we know and what should I do?
Features
Air pollution and me
What do we know and what should I do?
Features
Dr Abigail Whitehouse, Centre for Genomics and Child Health, Queen Mary University of London, UK
https://doi.org/10.36866/122.30
With the current results of an inquest into the role of air pollution in a child’s death from asthma, air pollution and its health effects once again return to the forefront of mainstream media. The media brings the research to life with snippets of studies demonstrating effects from not only cars and industries, but also our home cooking habits. With the levels in the UK exceeding WHO guidance year on year, the focus now moves to what we can do about it. In order to answer this, we need to answer the question, what does air pollution actually do to our bodies and therefore what approaches are best taken to address the current crisis? In this article we will cover the health impacts of air pollution and how they may occur and touch upon ways to combat pollution exposure.
What is air pollution?
Air pollution is the presence in the air of a substance that has harmful or poisonous effects on living beings. Its sources vary depending on where you are in the country or the world, but they fall into two main categories: indoor and outdoor. Outdoor pollutants are primarily:
• Particulate matter (PM) – soot, smog, dust, with a carbon centre. These can be natural (such as sand from the Saharan desert), but typically come from combustion sources such as traffic-related air pollution (TRAP) from cars and lorries, and industrial processes.
• Nitrogen oxides (NOx)– gases generated by vehicles through combustion processes in the air. These gases are highly interactive with PM and often sit on their surfaces. The health impacts of exposure are closely linked to (and at times indistinguishable from) PM.
• Ozone (O₃) – formed when other pollutants (such as NOx) react in sunlight.
Indoor air pollution is becoming increasingly important in the UK and includes second- hand cigarette smoke, carbon monoxide (CO) and carbon dioxide (CO₂) from open fires and gas hobs, biological allergens (house dust mites and moulds) and our roast dinners and toast (specifically the fine particles released through the process of cooking and using gas hobs).
How does air pollution get into the body?
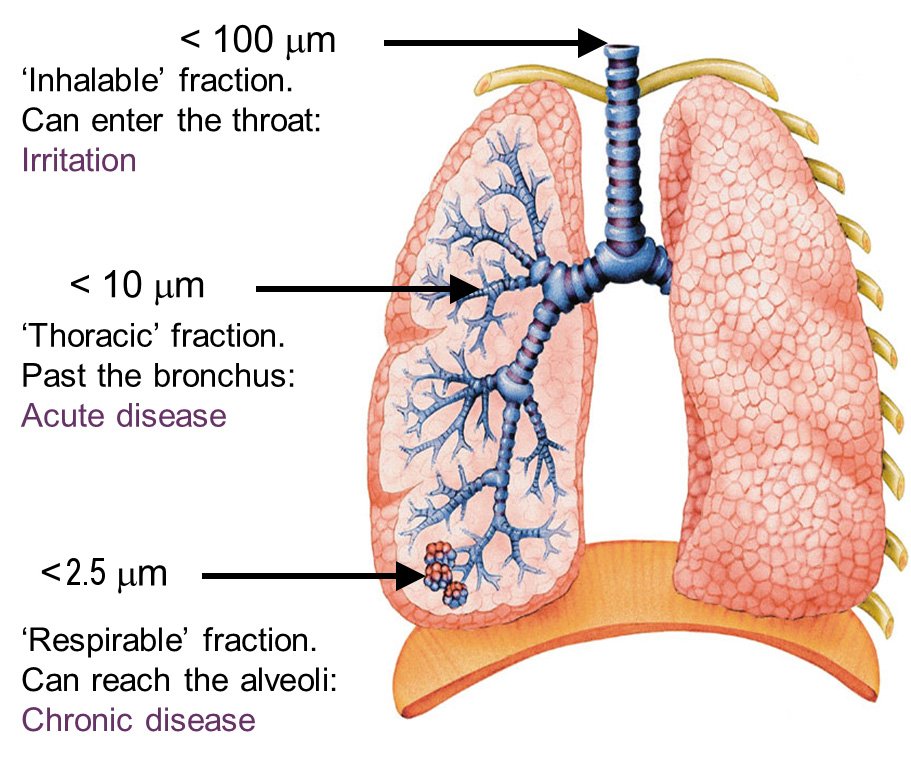
This is relatively straightforward – we breathe it in and this is where the size of PM becomes important. Particles between 5 and 10 microns (PM₁₀ but not PM₂.₅) are most likely to be found in the tracheobronchial tree (the bigger upper airways), whereas small particles are more likely to penetrate further, even as far as the alveoli where gas exchange takes place (Fig. 2).
What happens to PM once it is in the lungs?
What happens after we breathe the pollutants in is the part where research is still taking place but there are some pathways that are becoming clear.
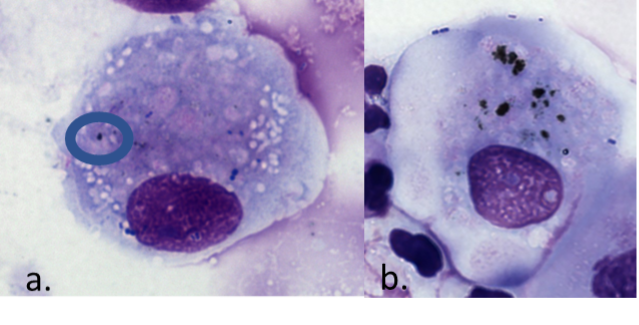
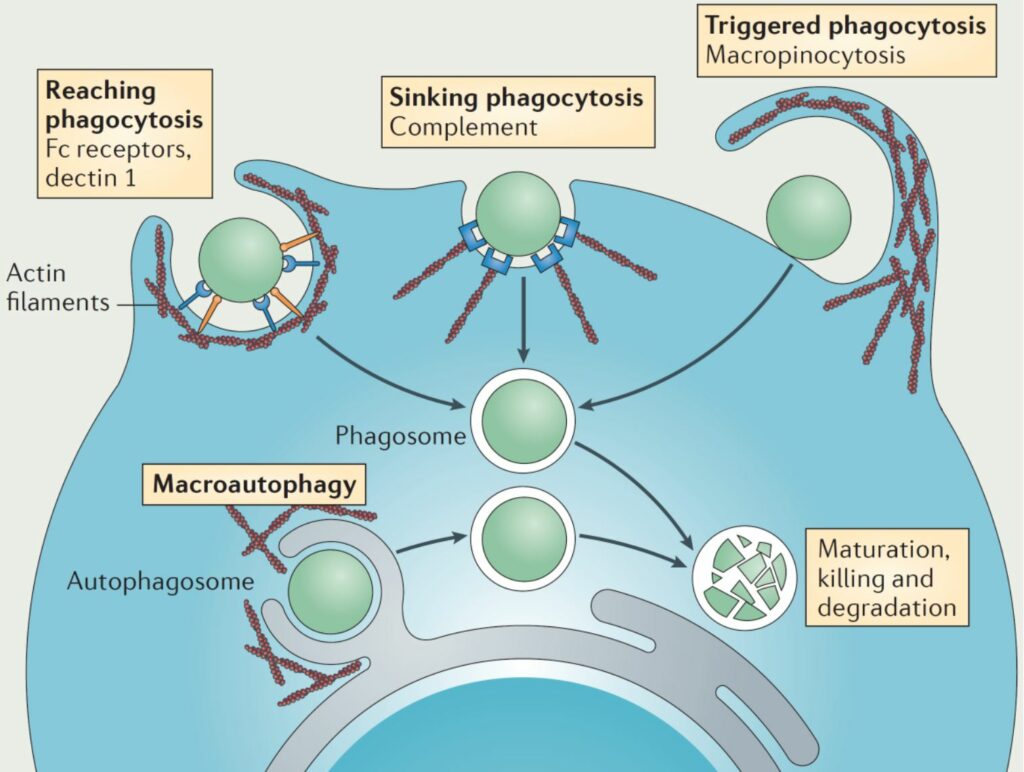
Once PM and carbon particles make it into the lungs they are met with the frontline cells of the immune system, specifically macrophages. Macrophages are phagocytes, they sit in the alveoli and on the epithelium, and when the PM arrives, they engulf it and initiate an inflammatory signalling pathway and cell cascade (Sijan et al., 2015). This is confirmed by the ability to see carbon within airway macrophages (either collected by induced sputum or bronchoalveolar lavage) (Fig. 3).
This is clinically important. Multiple studies have found that not only does airway macrophage black carbon (AMBC) correlate with external markers of pollution exposure (modelled or personal monitoring) (Bai et al., 2015) but also that it correlates with health effects. For example, Kulkarni et al. demonstrated an inverse correlation between AMBC and lung function in healthy children, where children with higher levels of AMBC have reduced FEV₁ (forced expiratory volume in 1 second) (Kulkarni et al., 2006). These data are compatible with studies that have shown reduced lung function in children exposed to higher levels of air pollution such as in California where pollution is high (Gauderman et al., 2002). Similarly, adults arriving from higher polluted cities from across the world outside of Belgium had significantly higher AMBC and lower lung function when compared with adult long- term residents of Belgium, where levels are relatively lower (Bai et al., 2018).
regulatory T cell formation) state to an increased inflammatory state (resulting in a switch towards T helper type 2 cells), such as that seen in asthma. DCs are affected or influenced by what they are exposed to, with exposure to heavy metals, particulate matter or cigarette smoke all altering the function and maturation potential (and therefore the subsequent T-cell responses) of these cells (Pfeffer et al., 2018).
So, what does air pollution do to health?
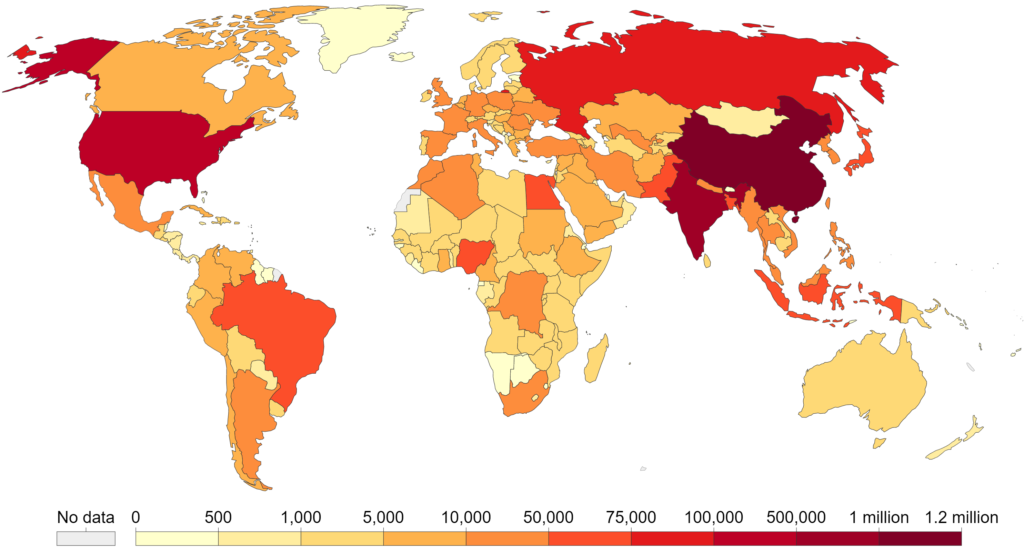
Air pollution exposure is the fifth leading risk factor for mortality worldwide with estimates of yearly attributable deaths now at 6.67 million (see Fig. 1; nearly 12% of the global total (Health Effects Institute, 2020). The physiological impact of exposure to pollutants can be seen throughout the life course, from the fetus to old age, and we now know that they affect almost every bodily system, with the respiratory system being the most obviously affected. Exposure to NOx and PM has significant effects on both lung development and lung function, with the effects starting in utero when the fetus is “indirectly” impacted due to placental insufficiency, a process in which the placenta is unable to provide adequate support to the growing fetus (van den Hooven et al., 2012). Subsequently this results in adverse birth outcomes such as low birth weight and preterm delivery (Ha et al., 2014), which are associated with PM exposure. These will affect lung growth and development and may have long-lasting impacts such as a predisposition to chronic lung diseases in later life.
Lung function has often been used as a marker of pollution exposure, with significant impacts on both FEV₁ and FVC (forced vital capacity) negatively affected by PM and NOx/NO₂ exposure (Hwang et al., 2015; Tager et al., 2005). When exposure occurs in childhood, those affected may never achieve optimum lung function potential for their height and sex. The Children’s Health Study found that the estimated proportion of 18-year-old subjects with a low FEV₁ (defined as a ratio of observed to expected FEV₁ of less than 80 percent) was 4.9 times as great at the highest level of exposure to PM₂.₅ as at the lowest level of exposure across the studied areas in California (Gauderman et al., 2004), which will then result in greater declines in adulthood.
Further health effects include exacerbation of existing cardiovascular disease and increased risk of myocardial infarctions, heart failure and stroke. There is significant evidence that pollution is associated with cancer and there is emerging evidence that exposures may also contribute to type 2 diabetes, Alzheimer’s disease and potentially autism incidence.
Well, what should we do?
With overwhelming evidence of harm, now is the time to declare that our priority is to reduce air pollution exposure, particularly for those most as risk, children. It is clear that to reduce exposure a buy-in from governments and policy makers is required, to increase funding for pollution-lowering policies such as low emission zones and bans on polluting vehicles. However, large-scale interventions will take time to have impact, so we need to promote small-scale pollution- reducing strategies that we can do in our own homes (more research is needed to look at effectiveness of these). Similarly, we need to promote how to reduce our own exposure through avoiding pollution hot-spots and increasing time spent in green spaces. Now is the perfect time to start, pollution levels were significantly affected by the coronavirus lockdown in the UK, with significant reductions noted by Defra of a 40% reduction in NOx levels. However, they are already returning to pre-lockdown levels.
References
Bai Y et al. (2018). Carbon load in airway macrophages as a biomarker of exposure to particulate
air pollution; a longitudinal study of an international Panel. Particle and Fibre Toxicology 15, 14. https://doi.org/10.1186/s12989-018-0250-8
Bai Y et al. (2015). Carbon loading in airway macrophages as a biomarker for individual exposure to
particulate matter air pollution – A critical review. Environment International 74, 32–41. https://doi.org/10.1016/j.envint.2014.09.010
Gauderman WJ et al. (2004). The effect of air pollution on lung development from 10 to 18 years of
age. New England Journal of Medicine 351, 1057–1067. https://doi.org/10.1056/NEJMoa040610
Gauderman WJ et al. (2002). Association between air pollution and lung function growth in southern California children: results from a second cohort. American Journal of Respiratory and Critical Care Medicine 166, 76–84. https://doi.org/10.1164/rccm.2111021
Ha S et al. (2014). The effects of air pollution on adverse birth outcomes. Environmental Research 134, 198–204. https://doi.org/10.1016/j.envres.2014.08.002
Hwang BF et al. (2015). Relationship between exposure to fine particulates and ozone and reduced
lung function in children. Environmental Research 137, 382–390. https://doi.org/10.1016/j.envres.2015.01.009
Kulkarni N et al. (2006). Carbon in airway macrophages and lung function in children. New England Journal of Medicine 355, 21–30. https://doi.org/10.1056/NEJMoa052972
Lin W et al. (2013). Meta-analysis of the effects of indoor nitrogen dioxide and gas cooking on asthma and wheeze in children. International Journal of Epidemiology 42, 1724–1737. https://doi.org/10.1093/ije/dyt150
Macintyre EA et al. (2014). Air pollution and respiratory infections during early childhood: an analysis of 10 European birth cohorts within the ESCAPE Project. Environmental Health Perspectives 122, 107–113. https://doi.org/10.1289/ehp.1306755
Pfeffer PE et al. (2018). Urban particulate matter stimulation of human dendritic cells enhances priming of naive CD8 T lymphocytes. Immunology 153, 502–512. https://doi.org/10.1111/imm.12852
Sijan Z et al. (2015). An in vitro alveolar macrophage assay for the assessment of inflammatory cytokine expression induced by atmospheric particulate matter. Environmental Toxicology 30, 836–851. https://doi.org/10.1002/tox.21961
Tager IB et al. (2005). Chronic exposure to ambient ozone and lung function in young adults. Epidemiology 16, 751–759. https://doi.org/10.1097/01.ede.0000183166.68809.b0
Van Den Hooven EH et al. (2012). Air pollution exposure and markers of placental growth and function: the generation R study. Environmental Health Perspectives 120, 1753–1759. https://doi.org/10.1289/ehp.1204918
