
Physiology News Magazine
Can a single bout of exercise prevent decompression sickness?
A single session of high-intensity exercise may form the basis for a novel approach to greatly reducing the risk of decompression sickness
Features
Can a single bout of exercise prevent decompression sickness?
A single session of high-intensity exercise may form the basis for a novel approach to greatly reducing the risk of decompression sickness
Features
Ulrik Wisløff (1,2*), Russell S. Richardson (1,3), Zeljko Dujic (4), Alf O. Brubakk (1)
1: Department of Circulation and Medical Imaging, Norwegian University of Science and Technology
2: Department of Cardiology, St. Olavs Hospital, Trondheim, Norway, Faculty of Medicine, Medical Technology Center, Trondheim, Norway
3: Department of Medicine, University of California San Diego, La Jolla, CA, USA
4: Department of Physiology and Biophysics, University of Split School of Medicine, Split, Croatia
ulrik.wisloff@medisin.ntnu.no
https://doi.org/10.36866/pn.55.16

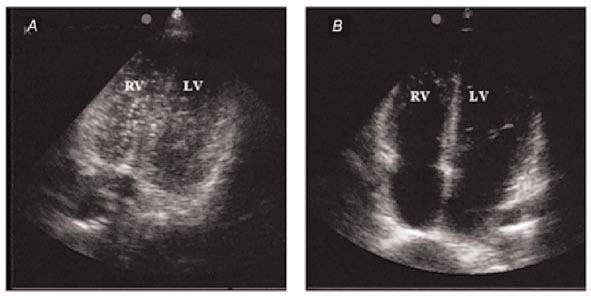
Decompression sickness (DCS) following diving, during un-pressurized aircraft flight or space flight extravehicular activity is believed to be initiated by the formation of gas bubbles in the tissue and blood. Nitrogen dissolves in the blood during dives, but comes out of solution if divers return to normal pressure too rapidly – like bubbles coming out of champagne when the bottle is uncorked. The predominant theory is that bubbles grow from preformed nuclei composed of small (approx. 1 micron) stable gas bubbles (Yount & Strauss, 1982). Nitrogen bubbles may cause effects ranging from skin rashes to seizures, coma and death. Even though the risk of DCS is minimized by changing the composition of the gas that is breathed and gradual decompression, DCS can still occur unpredictably. Exercise has long been considered an additional risk factor for DCS, but recent studies in our laboratory (Wisløff & Brubakk, 2001; Wisløff et al. 2003; Wisløff et al. 2004; Dujic et al. 2004) indicates that this notion needs updating.
During diving, gas must be breathed at ambient pressure and tissue equilibrates with the elevated inspired inert gas partial pressure forming a reservoir for bubble growth; with exercise, tissues that receive increased blood flow equilibrate more rapidly. By a separate mechanism, exercise following diving or shortly before or after decompression to altitude can promote bubble formation (e.g. Dervay et al. 2001). Exercise during the days preceding diving has received little attention. There are three animal studies (mice, pigs and rats) and all reveal that several weeks of daily aerobic training dramatically reduces the incidence of severe DCS (e.g. Wisløff & Brubakk, 2001). These studies have postulated rheological changes that alter the susceptibility to DCS, modified tissue perfusion, and reduced body fat (in which nitrogen is more soluble). None of these mechanisms are convincing, particularly in light of the findings that a single bout of exercise is equally effective as a longer training regimen and produces a short-term (1-2 days) reduction in decompression-induced bubble formation (Wisløff & Brubakk, 2001).
‘Good’ and ‘bad’ exercise?
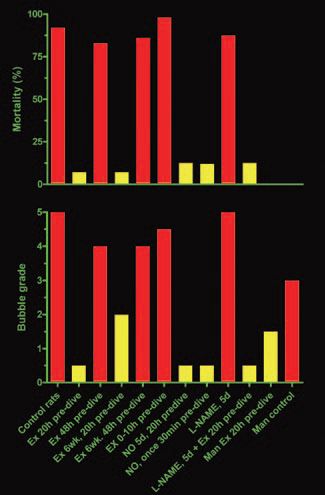
Initially we found that nitrogen bubbles only formed in the blood of unfit rats. However, by chance we noticed that one bout of exercise 20 h prior to the dive was just as beneficial as 6 weeks of exercise training. Fit rats sent on dives 2 days after stopping exercise developed as many bubbles as unfit rats. Thus, there was no beneficial effect of pre-dive exercise if the exercise was performed too close (e.g. 0.5h, 5h and 10 h), or too far in advance (e.g. 48 h) of the dive time (Wisløff et al. 2004). Furthermore, in agreement with Dervey et al. (2001), unpublished results from our laboratory suggest that exercise immediately prior to a dive promotes bubble formation. Thus, there seems to be ‘good’ exercise and ‘bad’ exercise. Recently we confirmed that a single bout of strenuous exercise 24 h before a dive to 18 m of seawater significantly reduced the average number of bubbles in the pulmonary artery in man, and that there was no correlation between aerobic capacity and amount of bubble formation (Dujic et al. 2004). Preliminary data from our laboratory also indicate that only strenuous exercise has a protective effect.
Mechanisms
We currently think that nitric oxide (NO) influences bubble formation and thus is involved in the development of DCS. The body produces NO during exercise; it is crucial for regulating breathing and blood flow, and there is evidence that NO ’makes the inner surface of blood vessels more slippery‘. Nitrogen bubbles are seeded like crystals on rough surfaces: the smoother the blood vessels, the harder it is for bubbles to form. If the NO-production is blocked we observe a substantial increase in bubble formation; however, exercise still gives protection despite NO-blockade, suggesting that there is more than just NO involved. Furthermore, both chronic and acute administration of an NO-donor protects against bubble formation and death in rats (Wisløff et al. 2003; 2004) without performing exercise. We speculate that both exercise and NO hinder bubble formation via alterations in vascular endothelial properties since preexisting gas nuclei are probably attached to the endothelium, where they grow into bubbles that are dislodged into the blood stream. However, if the mechanism of exercise-induced suppression of bubble formation is related solely to nitric oxide production, then the timing of NO administration in relation to its prophylactic effects on bubble formation might be expected to be similar. We recently reported (Wisløff et al. 2004) that administration of an NO-releasing agent reduced bubble formation even when given 30 min prior to hyperbaric exposure (without any exercise). Thus, the timing of the responses to exercise and NO administration were quite different (as exercise just prior to a dive was ‘bad exercise’), indicating that it is probably not NO alone that results in the exercise-induced protection.
An alternative explanation is that exercise may have a direct effect on micronuclei. Exercise before decompression can enhance bubble formation, but the effect is only temporary, decaying with a half-life of approximately 1 h in humans (Dervay et al. 2002). It is likely that micronuclei are activated but the resulting micro-bubbles dissolve if decompression does not occur during their lifetime. Since only a fraction of dissolving bubbles decay into gas micronuclei that can be reactivated into bubbles, it is possible that exercise without decompression depletes the population of micronuclei. Regeneration of the primordial micronuclei population may take 10-100 h (Yount, 1982), and this could explain the temporary protection against bubble formation.
Concluding remarks
Whether or not the effect of exercise on bubble formation operates through the formation of NO as we hypothesize, or through yet another mechanism, the present studies significantly advance our understanding of the effects of pre-dive exercise, and provide another means of ameliorating the formation of bubbles upon decompression in humans.
Since bubble formation is associated with decompression sickness, the studies (Wisløff & Brubakk 2001; Wisløff et al. 2003; 2004; Dujic et al. 2004) may impact broadly on the field of diving physiology. This work potentially effects a large number of the world’s population; in addition to pilots and diving professionals who are at risk of DCS as a consequence of occupation, there are an estimated 854,000 new certifications for SCUBA divers issued worldwide each year.
At this point our data indicate that both timing of exercise and exercise intensity is critical. Before pre-dive exercise can be widely adopted as a predictable safeguard against DCS we will need further standardization and studies. For instance, we need a better understanding of how much exercise is necessary to provide a given degree of protection, and we must develop tools to tell whether we are protected or not before diving. The understanding of the mechanisms involved is, in our opinion, critical as this may ultimately allow us to prevent DCS by biochemical means.
References
Dervay JP, Powell MR, Butler B, & Fife CE (2002). The effect of exercise and rest duration on the generation of venous gas bubbles at altitude. Aviat Space Environ Med 73, 22-27.
Wisloff U & Brubakk AO (2001). Aerobic endurance training reduces bubble formation and increases survival in rats exposed to hyperbaric pressure. Journal of Physiology, 537, 607 – 611.
Dujic Z, Duplancic D, Marinovic-Terzic I, Bakovic D, Ivancev V, Valic Z, Eterovic D, Petri N, Wisloff U, Brubakk AO (2004). Aerobic exercise before diving reduce venous gas bubbles formation in human. J Physiol. 555: 637-642
Wisloff U, Richardson RS, Brubakk AO (2004). Exercise and nitric oxide prevent bubble formation: A novel approach to the prevention of decompression sickness? J Physiol. 555: 825-829
Wisloff U, Richardson RS, Brubakk AO. (2003). NOS inhibition increases bubble formation and reduces survival in sedentary but not exercised rats. J Physiol. 546: 577-82.
Yount D & Strauss R (1982). On the evolution, generation and regeneration of gas cavitation nuclei. J Acoust Soc AM 65, 1431-1439.
Yount D (1982). Journal of the Acoustical Society of America 71, 1473-1481
News flash
The original manuscripts discussed in this article and a Perspectives article relating to them, published in The Journal of Physiology (555, 637-642, 825-829 and 588), formed the basis of the first press release circulated by the Society’s new publisher Blackwell Publishing.
This resulted in articles in New Scientist (27 March, p 12) and two online journals – Medical News Today (http://www.medicalnewstoday.com) and WebMDHealth (http://my.webmd.com)
