
Physiology News Magazine
Exercise is a good habit for bowel health
Features
Exercise is a good habit for bowel health
Features
Ozgur Kasimay & Berrak Ç Yegen
Department of Physiology, Marmara University School of Medicine, Istanbul, Turkey
https://doi.org/10.36866/pn.68.21

A substantial body of evidence verifies the benefits of regular physical activity on physiological and psychological well-being. Mild and moderate physical activity is associated with a lower incidence of mortality from any cause, especially from heart disease. Physical activity is beneficial to health because it reduces the risk of cardiovascular and endocrine diseases, improves bone and muscle conditioning and lessens anxiety and depression (Bi & Triadafilopoulos, 2003). It also diminishes high blood pressure, metabolic disorders such as diabetes mellitus, colon and rectal cancers, estrogen-dependent cancers of the ovary, breast, and endometrium (Woods, 1998), osteoporosis and mental depression; moreover, it can improve the quality of life.
The impact of exercise on the gastrointestinal system can be either beneficial or harmful for the gastrointestinal tract (Bi & Triadafilopoulos, 2003), depending partly on training intensity. The occurrence of gastrointestinal symptoms such as heartburn, nausea, vomiting, abdominal cramps, diarrhea and gastrointestinal bleeding is common during vigorous sports, causing the athlete to limit performance by reducing exercise intensity or duration (Peters et al. 2001). On the other hand, regular exercise at a low intensity may have protective effects on the gastrointestinal tract. Mild physical activity reduces abdominal distension by increasing intestinal gas clearance and transit of intraluminal gas (Villoria et al. 2006). The combination of diet and exercise therapy is effective in protection against reflux, as gas retention during rest decreases with dietary fibers and physical exercise. In particular, regular exercise at low intensity may reduce the risk of gastrointestinal disorders such as gastrointestinal hemorrhage, inflammatory bowel disease, cholelithiasis, diverticular disease or constipation.
Lack of physical activity is closely related to the development of colon cancer. There is strong evidence that regular exercise not only reduces the risk of developing colon cancer by up to 50%, but it also lowers the risk of death from colon cancer. A cohort study of Swedish men demonstrated that leisure-time physical activity was inversely associated with colorectal cancer risk (Larsson et al. 2006). Similarly, a Danish cohort study that aimed to assess the association between leisure-time physical activity and incidence of cancer in the general population of adult men and women, showed a significant inverse relationship between vigorous physical activity and cancer of the ovary for physically active women, while vigorous activity was associated with a non-significant lower risk of colon cancer in men (Schnohr et al. 2005). These results support a role of physical activity in reducing the risk of colon, rectal and ovarian cancer.
Ulcerative colitis is an idiopathic inflammatory bowel disease (IBD) with diffuse, recurrent inflammation of the colon and rectum, which is predominantly characterized by cycles of acute inflammation, ulceration and bleeding of the colonic mucosa. There is a long history of observations suggesting that psychological stress contributes to the course of IBD (Maunder, 2005) and that chronic stress increases the severity of intestinal inflammation (Gulpinar et al. 2004). Considering the improvements in psychological outcomes (i.e., depression, anxiety, mood states) reached by habitual exercise (Byrne & Byrne, 1993), a number of studies has investigated the preventive effect of physical activity on IBD. Sonnenberg (1990) showed that sedentary and physically less demanding occupations were associated with a higher risk of inflammatory bowel disease than were physically more demanding occupations. Further-more, the results of a case control study comparing incidence rates of IBD showed a reduced risk for physically active patients with Crohn’s disease or ulcerative colitis. However, in another study active Crohn’s disease patients had a high risk (Klein et al. 1998). Suggested underlying mechanisms in this preventive effect were the stress-reducing effects of physical activity and changes in local neuro-immuno-endocrine effects (Loudon et al. 1999). In accordance with these studies, we demonstrated that physical activity attenuates the severity of the colonic inflammation by a neutrophil-dependent mechanism (Fig. 1, top panel), by attenuating the oxidative tissue damage, by reducing lipid peroxidation (Fig. 1, middle panel) and by enhancing the antioxidative enzyme activity on the oxidative injury of the colon (Kasimay et al. 2006). Our results also support the fact that depletion of colonic glutathione is one of the major factors permitting lipid peroxidation and subsequent colonic damage.
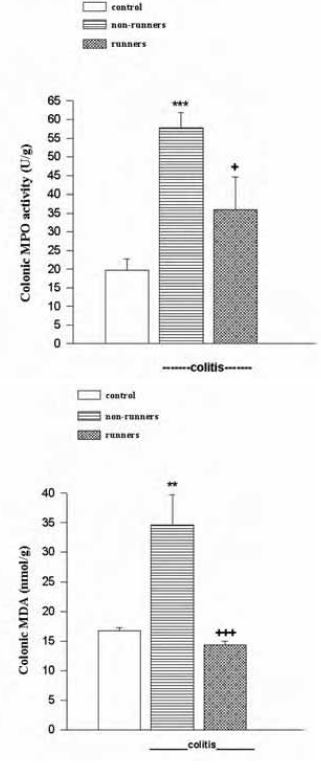
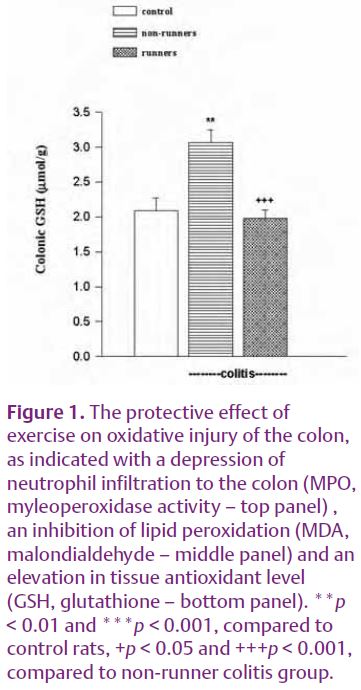
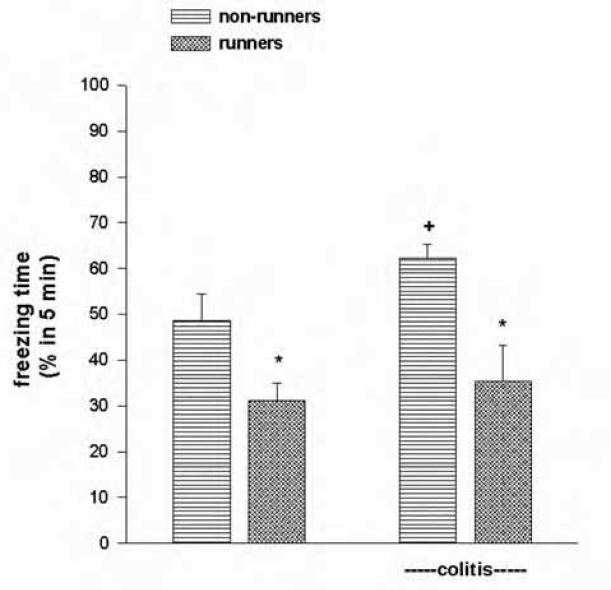
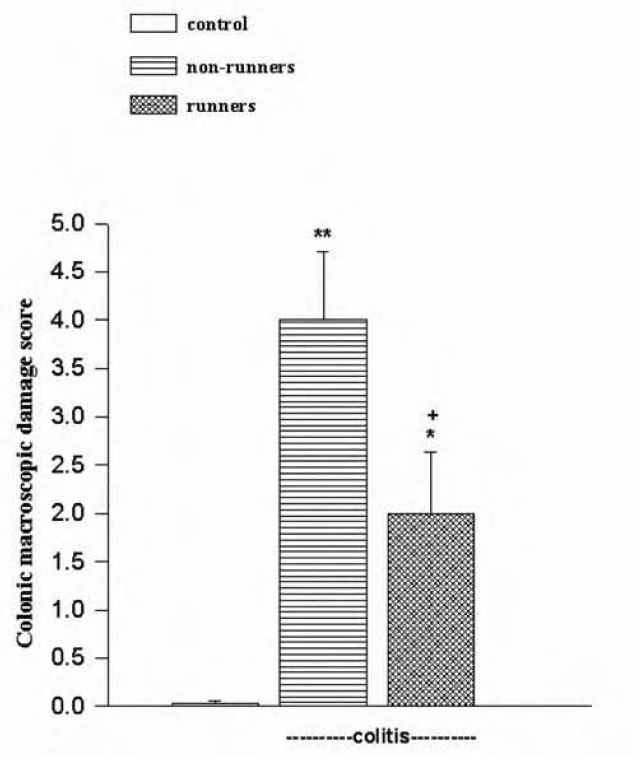
Since increased physical activity prevented colonic glutathione depletion, it appears that exercise supports the maintenance of antioxidant capacity in protecting the colonic tissue against oxidative stress (Fig. 1, bottom panel). Exercise-induced increases in aerobic fitness were shown to have beneficial short-term and long-term effects on psychological outcomes (DiLorenzo et al. 1999). Similarly, physical activity was postulated to reduce disease activity and perceived stress in IBD patients, while general well-being and quality of life were improved (Loudon et al. 1999). Among the possible explanations for psychological outcomes are the direct effects of neurotransmitters (e.g., serotonin) in the brain that function to elevate mood (McDonald & Hodgdon, 1991). We recently demonstrated that regular exercise attenuates the anxiety of stressed animals. However, in accordance with previous studies demonstrating that psychological stress might amplify intestinal inflammation (Collins, 2001), severity of colitis was enhanced as the level of anxiety was exaggerated. On the other hand, the degree of anxiety was reduced (Fig. 2) in regularly exercised rats that had significant attenuation of colonic inflammation (Fig. 3).
Exercise should be considered as a non-pharmacological intervention in controlling the course of inflammatory bowel diseases, specifically during stressful conditions that would trigger the exacerbation of the symptoms. In order to benefit from physical activity, including the health of the gut, people should perform moderate exercise at moderate intensity for 30 minutes/day at least 3 days/week. Regular exercise may not only help us attain a longer life, but also more years living independently with a better quality of life.
References
Bi L & Triadafilopoulos G (2003). Exercise and gastrointestinal function and disease: An evidence-based review of risks and benefits. Clin Gastroenterol Hepatol 1, 345–355.
Byrne A & Byrne DG (1993). The effects of exercise on depression, anxiety and other mood states: A review. J Psychosom Res 37, 565–574.
Collins SM (2001). Stress and the gastrointestinal tract-IV. Modulation of intestinal inflammation by stress: Basic mechanisms and the clinical relevance. Am J Physiol 280, G315–318.
DiLorenzo TM, Bargman EP, Stucky-Ropp R, Brassington GS, Frensch PA & LaFontaine T (1999). Long-term effects of aerobic exercise on psychological outcomes. Prev Med 28, 75–85.
Gulpinar MA, Ozbeyli D, Arbak S & Yegen BC (2004). Anti-inflammatory effect of acute stress on experimental colitis is mediated by cholecystokinin-B receptors. Life Sci 75, 77–91.
Kasimay O, Guzel E, Gemici A, Abdyli A, Sulovari A, Ercan F, Yegen BC (2006). Colitis-induced oxidative damage of the colon and skeletal muscle is ameliorated by regular exercise in rats: The anxiolytic role of exercise. Exp Physiol 91, 897–906.
References
Bi L & Triadafilopoulos G (2003). Exercise and gastrointestinal function and disease: An evidence-based review of risks and benefits. Clin Gastroenterol Hepatol 1, 345–355.
Byrne A & Byrne DG (1993). The effects of exercise on depression, anxiety and other mood states: A review. J Psychosom Res 37, 565–574.
Collins SM (2001). Stress and the gastrointestinal tract-IV. Modulation of intestinal inflammation by stress: Basic mechanisms and the clinical relevance. Am J Physiol 280, G315–318.
DiLorenzo TM, Bargman EP, Stucky-Ropp R, Brassington GS, Frensch PA & LaFontaine T (1999). Long-term effects of aerobic exercise on psychological outcomes. Prev Med 28, 75–85.
Gulpinar MA, Ozbeyli D, Arbak S & Yegen BC (2004). Anti-inflammatory effect of acute stress on experimental colitis is mediated by cholecystokinin-B receptors. Life Sci 75, 77–91.
Kasimay O, Guzel E, Gemici A, Abdyli A, Sulovari A, Ercan F, Yegen BC (2006). Colitis-induced oxidative damage of the colon and skeletal muscle is ameliorated by regular exercise in rats: The anxiolytic role of exercise. Exp Physiol 91, 897–906.
Klein I, Reif S, Farbstein H, Halak A & Gilat T (1998). Pre-illness non dietary factors and habits in inflammatory bowel disease. Ital J Gastroenterol Hepato 30, 247–251.
Larsson SC, Rutegard J, Bergkvist L, Wolk A (2006). Physical activity, obesity, and risk of colon and rectal cancer in a cohort of Swedish men. Eur J Cancer 42, 2590–2597.
Loudon CP, Corroll V, Butcher J, Rawsthorne P & Bernstein CN (1999). The effects of physical exercise on patients with Crohn’s disease. Am J Gastroenterol 94, 697–703.
Maunder RG (2005). Evidence that stress contributes to inflammatory bowel disease: Evaluation, synthesis, and future directions. Inflamm Bowel Dis 11, 600–608.
McDonald DG & Hodgdon JA (1991). Psychological effects of aerobic fitness training: Research and therapy. Springer-Verlag, New York.
Peters HP, De Vries WR, Vanberge-Henegouwen GP, Akkermans LM (2001). Potential benefits and hazards of physical activity and exercise on the gastrointestinal tract. Gut 48, 435–439.
Schnohr P, Gronbaek M, Petersen L, Hein HO & Sorensen TI (2005). Physical activity in leisure-time and risk of cancer: 14-year follow-up of 28,000 Danish men and women. Scand J Public Health 33, 244–249.
Sonnenberg A (1990). Occupational distribution of inflammatory bowel disease among German employees. Gut 31, 1037–1040.
Villoria A, Serra J, Azpiroz F, Malagelada JR (2006). Physical activity and intestinal gas clearance in patients with bloating. Am J Gastroenterol 101, 2552–2557.
Woods JA (1998). Exercise and resistance to neoplasia. Can J Physiol Pharmacol 76, 581–588.
