Physiology News Magazine
Helping the most vulnerable survive heatwaves today and in the future
Using physiology to identify cooling interventions that work
Features
Helping the most vulnerable survive heatwaves today and in the future
Using physiology to identify cooling interventions that work
Features

https://doi.org/10.36866/pn.127.29
Professor Ollie Jay
Heat and Health Research Incubator, University of Sydney, Australia
For several days in July 2022, people across the United Kingdom and the rest of Europe tasted a sample of the future effects of climate change. Peak temperatures (measured in the shade) exceeded 40˚C in the UK for the first time in recorded history, while the mercury soared beyond 45˚C in some parts of mainland Europe. This weather follows a string of record-breaking heatwaves in South Asia from March to May where in highly populated cities such as New Delhi, residents suffered through 5 heatwaves in 8 weeks, the fiercest of which peaked at 49.2˚C.
The devastating effects of extreme heat on human health are clear. Heatwaves are already responsible for more deaths than all other natural disasters (Gasparrini et al., 2015). The legacy of human activity over the past century means more intense and frequent heatwaves are all but assured for at least the remainder of this century. While epidemiologists have provided important information on the subgroups of society that are most at risk of the negative health effects of extreme heat, physiologists can provide essential insight into a) why some people are more intolerant than others to extreme heat exposure, and b) the types of interventions that can be used to increase extreme heat resilience of the most vulnerable.
Adaptative capacity is key to coping with heatwaves
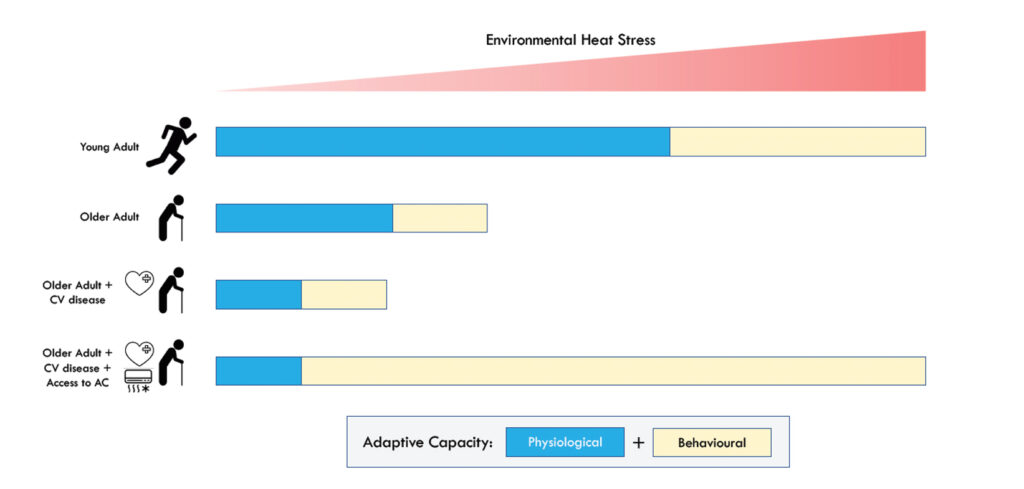
The ability to safely endure a heatwave is dependent on the combined physiological and behavioural capacity to adapt to extremely hot environments (Fig.1). From a physiological perspective, age-related decrements in both sudomotor function (i.e. autonomic nervous system control of sweat gland activity) and levels of cutaneous vasodilation compromise the ability to regulate body temperature in the heat (Kenney and Munce, 2003), and thus elevate heatstroke risk. Emerging evidence indicates that these thermoregulatory ageing effects may be further compounded by the presence of chronic diseases such as diabetes (Kenny et al., 2016). People with pre-existing heart conditions are at a heightened risk of heat-related morbidity and mortality, but not necessarily due to critically high body temperatures. The most likely mechanistic pathway is a compromised capacity to tolerate the elevated cardiovascular strain that evolves with the greater cardiac output required to maintain blood pressure upon the large reductions in total peripheral resistance caused by heat-induced cutaneous vasodilation (Ebi et al., 2021). Heat stress risk is also exacerbated in people who are excessively exposed to extreme heat because of a low behavioural adaptive capacity. Air-conditioning (AC) use offers exceptional protection against heat-related illnesses in a heatwave (Bouchama et al., 2007), and it is now the leading heat coping strategy globally. Yet, because of high capital and operational costs, AC is often inaccessible to people living with poverty who subsequently rank highest among the most vulnerable. People with disabilities, especially those living in isolation, may lack mobility and be unable to engage fully in heat-avoidance behaviour. The heat-health effects of these factors are further aggravated by residing in housing constructed of low-cost materials with poor thermal performance, especially if situated in densely built urban settings, where heat exposure is further amplified by the urban heat island effect.
The search for cooling alternatives to AC in heatwaves
Identifying simple and accessible cooling strategies that can be adopted by those with both a low physiological and behavioural capacity to adapt to extreme heat is a high priority for optimising public health preparedness in advance of an impending heatwave disaster. Electric fan use has been widely considered as an attractive option. They are cheap to purchase, consume less than one-twentieth of the electricity required to operate AC, are simple to use, and widely available. The effectiveness of electric fans for cooling in heatwave conditions though has been contentious for decades. In the 1990s, fan distribution programmes targeted the most vulnerable in cities such as New York and Chicago as part of their heatwave management strategy. But these programmes were discontinued due to concerns that fans paradoxically increase the risk of heat-related illnesses. In fact, most major public health agencies (e.g. WHO, CDC) now insist that fans should not be used during heatwaves because they can supposedly “speed the onset” of heat exhaustion when used above 35˚C. Similarly, in their most recently issued heatwave guidance, the National Health Service in the UK (National Health Service, 2022) state that fan use above 35°C “may not prevent heat related illness”, “can cause excess dehydration”, and they should be placed “a certain distance from people, not aiming it directly on the body and to have regular drinks”. This is apparently “especially important in the case of sick people confined to bed”.
The notion that fan use may be detrimental in heatwave conditions most likely arises from the understanding that as air temperature exceeds skin temperature, which reaches ~35°C when fully vasodilated, more sensible heat will flow into the body with additional air movement. After all, this is the basis upon which fan assisted ovens accelerate cooking. However, unlike a lump of meat in an oven, humans secrete sweat on to the skin surface when heated and the subsequent evaporative heat loss serves to greatly cool the body.
Moreover, this evaporation can be massively enhanced with greater air velocities, leading to the evaporation of sweat that would otherwise either sit on the skin, or drip off the body altogether and provide no latent cooling. It is therefore clear that only when the additional sensible heat gain cannot be counterbalanced by greater evaporative heat loss will fans accelerate body heating. However, there are physiological limitations to sweating that will impact the efficacy of fan use (Jay et al., 2015). Age-related decrements in sweat output for example are progressively observed above the age of 60 years (Kenney and Munce, 2003), most notably on the forehead, face, and arms (Inoue et al., 1991). Furthermore, in arid conditions most sweat will freely evaporate even in relatively still air owing to the higher water vapour pressure gradient between the skin and environment, meaning that during very hot and dry heatwaves fan use may only generate minimal evaporative benefits while forcing additional heat into the body via convection. Notwithstanding the rationale described above, no empirical evidence seems to yet be available supporting 35˚C as a critical threshold beyond which fans do not help alleviate heat stress, or even worse, aggravate it. Indeed, a 2012 Cochrane review, which is often cited as supporting evidence for existing public health guidance on fan use, concluded “no evidence at all exists supporting or refuting the use of electric fans during heatwaves” (Gupta et al., 2012). It is also unclear what other personal-level cooling strategies can be used as alternatives. Actively wetting the skin with water should boost evaporative potential, while immersing limbs, which are highly vascularised and have a high surface area-to-volume ratio, in cold water could augment conductive heat transfer away from the body.
Using physiology to identify cooling interventions that work
Changes in the risk of heat-related illnesses can be inferred from the measurement of a triad of biomarkers of physiological heat strain. Rises in core temperature indicate the risk of hyperthermia, while measures of rate-pressure product (i.e. systolic blood pressure × heart rate) serve as an indicator of myocardial oxygen consumption and therefore cardiovascular strain, and rates of whole-body sweat losses determine dehydration risk. Under simulated heatwave conditions in climate chambers, physiologists can measure these variables in a variety of participants with different clinical profiles to systematically assess the potential cooling efficacy of personal-level interventions.
Using a humidity-ramp protocol, pioneered by the Noll Research Laboratory at Penn State University (Kenney and Zeman, 2002), to identify the critical environmental condition under which the physiological compensation of cardiovascular strain and thermal strain is no longer possible, we observed a protective effect of electric fan use at both 36˚C and 42˚C in young healthy adults – some 1˚C and 7˚C above the current NHS fan use threshold, respectively (Ravanelli et al., 2015). Specifically, elevations in cardiovascular and thermal strain occurred at a higher humidity at each temperature with fan use. When comparing absolute humidity thresholds, our young healthy participants experienced less physiological heat strain with a fan at 42˚C than they did without a fan at 36˚C.
We further assessed whether an expression of ambient conditions that combines the effects of temperature and humidity (i.e. heat index (HI) – which adjusts temperature to the value that would elicit the same thermal sensation as the prevailing conditions if absolute humidity was fixed at 1.6 kPa) should be used to recommend fan use in heatwaves (Morris et al., 2019a), as per the US Protection Agency who instruct people to turn off fans at an HI of 37˚C. During an acute exposure to hot/humid (40˚C, 50% RH) conditions with a high HI – representative of common heatwaves in temperate climates, e.g. Western Europe, North America (except Southwest), Eastern China, fan use reduced cardiovascular and thermal strain. Yet, in very hot/dry conditions with a lower HI – representative of heatwaves in arid climates, e.g. Middle East, South Asia, Australia, fans worsened physiological heat strain. The use of HI as a means of determining whether fans should be used or not is therefore not recommended.

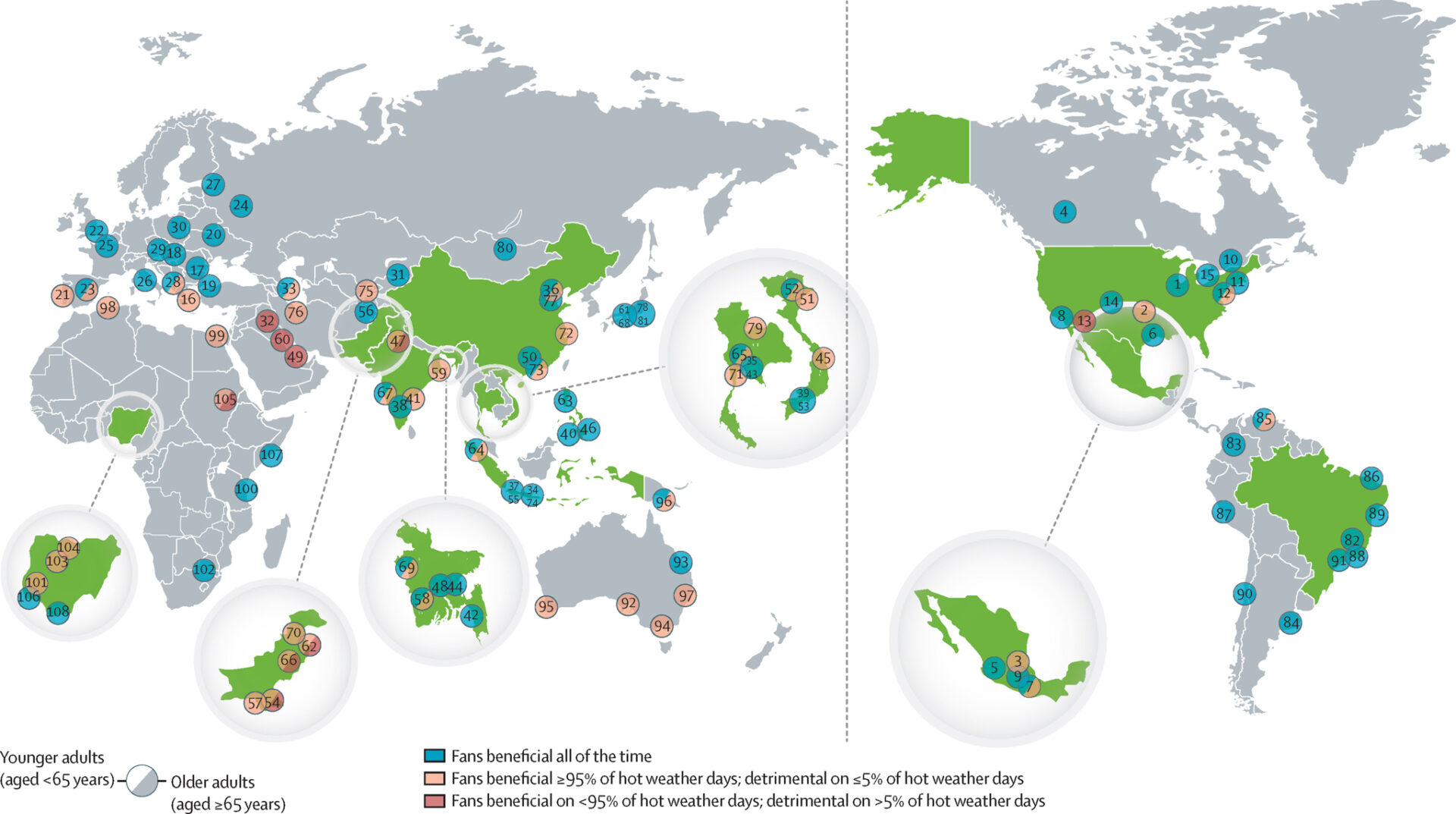
Importantly, these studies assessed the physiological responses of young healthy participants free from thermoregulatory impairments. Subsequent studies assessing fan use in older adults (>60 years) have shown that the beneficial effect of fan use is eliminated, and potentially reversed, at 42-43˚C (Gagnon et al., 2016; Cramer et al., 2020). Using biophysical modelling informed by these and other physiological data, we have subsequently proposed humidity dependent air temperature thresholds at which fans should not be used for healthy young adults, healthy older adults, and older adults taking prescription medications that interfere with sweating (Morris et al., 2021). While recognising that indoor temperature and humidity for a given set of outdoor conditions in a heatwave can vary, and be strongly affected by housing typology, providing historical heatwave conditions for context, we found that fan use should be almost universally recommended as an alternative cooling strategy in the UK, most of the rest of Europe, large swathes of Asia, North America, and South America (Fig.2). On the other hand, fans should be routinely discouraged in the Middle East due to high temperatures coupled with low humidity. Using these historical conditions, we also generated simplified fan-use temperature thresholds for public health messaging at which fan use would not be detrimental irrespective of humidity: 39˚C (young adults), 38˚C (healthy older adults), and 37˚C (older adults taking anticholinergic medication) (Jay et al., 2021).
The one concern by public health authorities about fan use in heatwaves that has been supported by physiological studies is accelerated dehydration. Despite smaller rises in core temperature, sweat rates are higher with fan use, most likely due to a higher skin temperature modifying the onset threshold and thermosensitivity of the sudomotor response (Ravanelli et al., 2020). However, practically this greater risk of dehydration can be offset with the ingestion of extra ~100-150 ml of water every hour.
When heatwave conditions exceed the thresholds for safe fan use, applying water to the skin using a spray bottle or sponge reduces heat-induced cardiovascular strain, improves thermal comfort, and slows the development of dehydration in heatwave conditions up to 47˚C (Morris et al., 2019b). Under the same conditions, the immersion of both feet in a bucket of cold tap water for 10 minutes every 20 minutes improves thermal comfort and reduces dehydration risk. Such interventions may potentially be useful for people living in very low resource environments without access to any electricity. They also provide an option as an emergency intervention for people during power outages, which have occurred with increasing regularity during heatwaves in recent years as more people turn to air conditioning and frail energy infrastructure has been unable to meet electricity demands with sufficient supply. The sustainable and accessible cooling strategies supported by the latest physiological evidence have been reported in our recent collaborative Lancet Series on Heat and Health (Jay et al., 2021) and are summarised in an infographic that is currently available in English (Fig.3), Spanish and Hindi.
The next steps
While these initial physiological studies provide a strong indication of sustainable and accessible cooling strategies that can be used to help the most vulnerable navigate safely through heatwaves, confirmation of their cooling efficacy in larger-scale studies is essential. This is particularly relevant for people with chronic diseases, such as cardiovascular disease, and over multi-day exposures in real-world heatwaves.
Any additional or multiplicative benefit from combining interventions, as well as interactions with chronic dehydration and different prescription medications also needs to be urgently assessed.
References
Bouchama A et al. (2007). Prognostic factors in heat wave related deaths: a meta-analysis. Archives of Internal Medicine 167, 2170-2176. https://doi.org/10.1001/archinte.167.20.ira70009
Cramer MN et al. (2020). Keeping older individuals cool in hot and moderately humid conditions: wetted clothing with and without an electric fan. Journal of Applied Physiology (1985) 128, 604-611. https://doi.org/10.1152/japplphysiol.00786.2019
Ebi KL et al. (2021). Hot weather and heat extremes: health risks. Lancet 398, 698-708. https://doi.org/10.1016/S0140-6736(21)01208-3
Gagnon D et al. (2016). Cardiac and thermal strain of elderly adults exposed to extreme heat and humidity with and without electric fan use. Journal of the American Medical Association 316, 989-991. https://doi.org/10.1001%2Fjama.2016.10550
Gasparrini A et al. (2015). Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet 386, 369-375. https://doi.org/10.1016/S0140-6736(14)62114-0
Gupta S et al. (2012). Electric fans for reducing adverse health impacts in heatwaves. Cochrane Database of Systematic Reviews 7, CD009888. https://doi.org/10.1002/14651858.cd009888.pub2
Inoue Y et al. (1991). Regional differences in the sweating responses of older and younger men. Journal of Applied Physiology 71, 2453-2459. https://doi.org/10.1152/jappl.1991.71.6.2453
Jay O et al. (2021). Reducing the health effects of hot weather and heat extremes: from personal cooling strategies to green cities. Lancet 398, 709-724. https://doi.org/10.1016/S0140-6736(21)01209-5
Jay O et al. (2015). Should electric fans be used during a heat wave? Applied Ergonomics 46 Pt A, 137-143. https://doi.org/10.1016/j.apergo.2014.07.013
Kenney WL, Munce TA (2003). Invited review: aging and human temperature regulation. Journal of Applied Physiology 95, 2598-2603. https://doi.org/10.1152/japplphysiol.00202.2003
Kenney WL, Zeman MJ (2002). Psychrometric limits and critical evaporative coefficients for unacclimated men and women. Journal of Applied Physiology (1985) 92,2256-2263. https://doi.org/10.1152%2Fjapplphysiol.00345.2020
Kenny GP et al. (2016). Body temperature regulation in diabetes. Temperature (Austin) 3, 119-145. https://doi.org/10.1080%2F23328940.2015.1131506
Morris NB et al. (2021). Electric fan use for cooling during hot weather: a biophysical modelling study. Lancet Planet Health 5, e368-e377. https://doi.org/10.1016/S2542-5196(21)00136-4
Morris NB et al. (2019a). The effects of electric fan use under differing resting heat index conditions: a clinical trial. Annals of Internal Medicine 171, 675-677. https://doi.org/10.7326/m19-0512
Morris NB et al. (2019b). A preliminary study of the effect of dousing and foot immersion on cardiovascular and thermal responses to extreme heat. Journal of the American Medical Association 322, 1411-1413. https://doi.org/10.1001/jama.2019.13051
UKHSA, NHS (2022). Heatwave plan for England: Protecting health and reducing harm from severe heat and heatwaves https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1096593/heatwave-plan-for-England-2022-5-August-2022.pdf
Ravanelli N et al. (2020). Steady-state sweating during exercise is determined by the evaporative requirement for heat balance independently of absolute core and skin temperatures. Journal of Physiology 598, 2607-2619. https://doi.org/10.1113/JP279447
Ravanelli NM et al. (2015). Heart rate and body temperature responses to extreme heat and humidity with and without electric fans. Journal of the American Medical Association 313, 724-725. https://doi.org/10.1001/jama.2015.153