
Physiology News Magazine
How good is spontaneous sequence analysis at measuring baroreflex sensitivity in man?
Spontaneous sequence analysis (SSA) is a widely used but controversial technique to measure sensitivity of the heart period component of the baroreflex in man. The principal controversy concerns whether all the sequences it finds are random or causal relationships between blood pressure and heart period. Evidence indicates that the data it generates are not substantially contaminated by random relationships. SSA therefore appears more useful than previously supposed and as good as (and no worse than) any other technique for measuring baroreflex sensitivity, but could still be improved.
Features
How good is spontaneous sequence analysis at measuring baroreflex sensitivity in man?
Spontaneous sequence analysis (SSA) is a widely used but controversial technique to measure sensitivity of the heart period component of the baroreflex in man. The principal controversy concerns whether all the sequences it finds are random or causal relationships between blood pressure and heart period. Evidence indicates that the data it generates are not substantially contaminated by random relationships. SSA therefore appears more useful than previously supposed and as good as (and no worse than) any other technique for measuring baroreflex sensitivity, but could still be improved.
Features
Michael Parkes
University of Birmingham, UK
https://doi.org/10.36866/pn.85.32

Introduction
The baroreflex is believed to be an important means of stabilising blood pressure in mammals and has multiple efferent components, including changes in heart rate, stroke volume and peripheral resistance. Systolic (rather than mean or diastolic) blood pressure (sPB) is usually measured as the input, since this represents the greatest dynamic stimulus to baroreceptors. Its heart rate component is the most often studied output, as it is easiest to measure and only this component is considered here. Mechanistically it may make more sense to consider heart period rather than heart rate (its inverse), since the control system actually advances or retards the next heart beat, rather than setting a particular heart rate.
No agreed gold standard for baroreflex sensitivity measurement.
A major problem in baroreflex sensitivity measurement is the absence of an agreed, absolute gold standard against which to validate all baroreflex sensitivity measurements. There are agreed absolute standards to measure pressure (mmHg) and time (milliseconds). But there is no agreement about how best to provoke the required change in pressure, how big the pressure change should be and over what time the heart period response should be measured. The absence of any accepted validation means there is no means of knowing what the hypothetically correct baroreflex sensitivity value should be when any technique is applied. So if two techniques agree on a baroreflex sensitivity value both could still be wrong. Conversely, if two techniques disagree, we don’t know which is right, or which is nearer the hypothetically correct value. Without validation, the next best thing is to establish whether each technique can identify the fundamental properties of the baroreflex in man. Perhaps the simplest fundamental property is the attenuation of the heart period component of the baroreflex by the inspiratory phase of the central respiratory rhythm (Mancia & Mark, 1983).
The first formal studies of the heart period component of the baroreflex in man used systemic injection of pressor or depressor drugs (phenylephrine, angiotensin II or nitroprusside) to cause a change in systolic blood pressure, measured the heart period response and derived a baroreflex sensitivity value in ms mmHg–1. This is sometimes called the ‘Oxford technique’. There are several reasons why not all accept this as the gold standard. Different drugs produce a different gain value and the gain value also differs (an hysteresis) depending on whether pressor or depressor drugs are used. Possibly both result from all drugs having other effects in addition to changing blood pressure. Furthermore, all apply an external stimulus to provoke the response, hence come up against Heisenberg’s Uncertainty Principle. The first proponents of the Oxford technique in man (Smyth et al. 1969) observed that the baroreflex was attenuated in inspiration. Indeed in this and later papers they suggested selecting only expiratory data for analysis.
Subsequent studies developed an alternative technique of applying suction or pressure around the neck. By changing arterial pressure in the neck this stimulates or unloads carotid baroreceptors. Again the heart period response is measured and a baroreflex gain value is calculated. This technique too encounters Heisenberg’s Uncertainty Principle and also alters only a sub-population of baroreceptors. It too detects inspiratory attenuation.
What is spontaneous sequence analysis?
An ingenious alternative idea in the 1980s exploited the fact that blood pressure is never constant, even in healthy, resting and recumbent subjects. It was proposed that, if the baroreflex operates continuously, these spontaneous changes in sBP could be taken as the input, and the output could be taken as heart periods at specific times (lags) in relation to the systolic pressure changes. Although initially using arterial catheters to measure pressure, this technique cleverly exploited the availability of servo-controlled sphygmomanometers (such as the FINAPRES) to track arterial pressure in the finger at around 100 Hz. The great attraction of combining SSA with the FINAPRES is that it provides a non-invasive technique (using only spontaneous physiological variations in pressure as the input) and therefore does not encounter Heisenberg’s Uncertainty Principle. It can also be used to test whether the hysteresis is a drug-induced artefact or a fundamental property of the baroreflex.
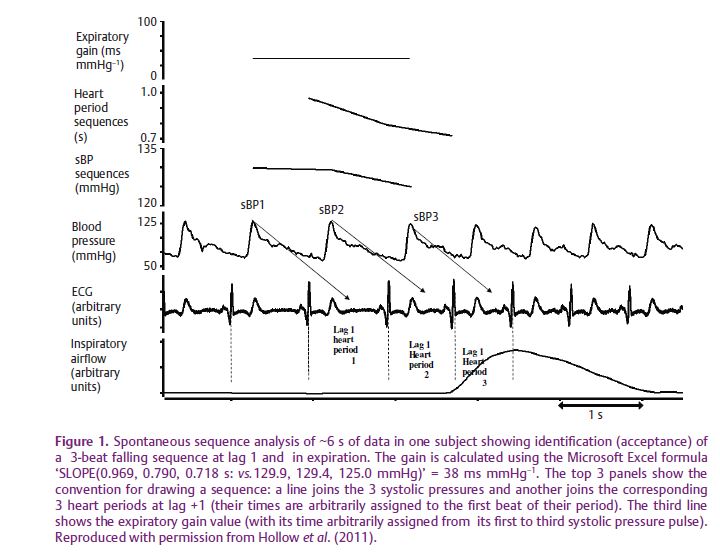
All that SSA requires is to record pressure and heart period with sufficient resolution and over a sufficiently long period. A computer programme then goes through the record one beat at a time to find the acceptable sequences. SSA makes the simplistic assumption that each sBP value influences only the next heart period. (More sophisticated analyses of the influence of sBP on multiple successive heart periods have yet to be explored.) For SSA the minimum number of sequential beats over which gain can be measured is three (it being impossible not to draw a straight line through only two data points). Three-beat sequences are also the most common sequence length found and, although longer sequences also occur, they are much less frequent and it is unclear what advantage they offer. Figure 1 shows how the programme searches either for the first three consecutive beats of rising systolic pressure accompanied by three increasing (lengthening) heart periods at a specified lag, or for three falling systolic pressures with three falling (shortening) periods. When found (accepted) their regression slope is calculated to derive the baroreflex sensitivity value in ms mmHg–1. If the first three beats do not meet these criteria, the programme then moves along one beat and searches again (with no beat being double counted). Finally, the mean gain value is calculated from as many accepted sequences as are found in the recording period.
The SSA controversy
As anybody who has tried to publish SSA data knows, use of the SSA technique is still highly controversial. There is no doubt that injection of sufficient drug, or a sufficient change in neck pressure, will cause systolic pressure changes that must cause a heart period response. With SSA, however, there is no means of distinguishing random from causal associations between spontaneous pressure changes and the heart period ‘responses’. Some believe that so many of these associations must be random that the mean gain value derived by SSA is meaningless. Undoubtedly some spontaneous sequences must be random, so the key questions are ‘how many?’ and ‘do they matter?’.
These can be addressed in a number of ways. The answers appear to be ‘not many’ and ‘probably not!’.
First, if all accepted sequences were random, then sinoaortic denervation should make no difference to the number of accepted sequences found nor to the mean gain value. Such experiments cannot be performed on man, but in several species of unanaesthetised animals sinoaortic denervation does make a large difference: the number of accepted sequences falls by at least 90% and their mean gain value tends to zero. This confirms that some spontaneous sequences are undoubtedly random, but shows that they form <10% of all sequences and appear to make no important contribution to the overall gain value.
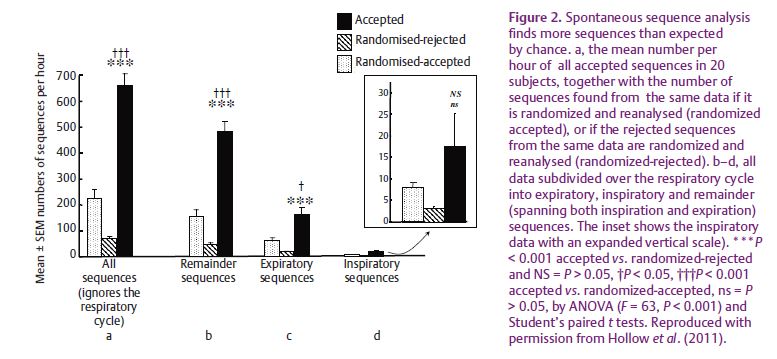
Second, if all accepted sequences were random, then SSA should find no more sequences than expected by chance (i.e. when using a random number generator to redistribute the original pressures and periods over time and then reanalysing this randomized data). A number of studies in man show, however, that SSA finds many more sequences than expected by chance (Fig. 2).
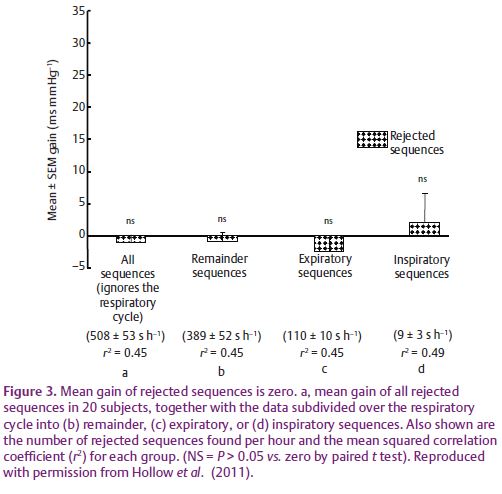
Third, we would expect the sequences rejected by SSA to be random and therefore their mean gain should be zero. We confirm (Fig. 3) that this is the case.
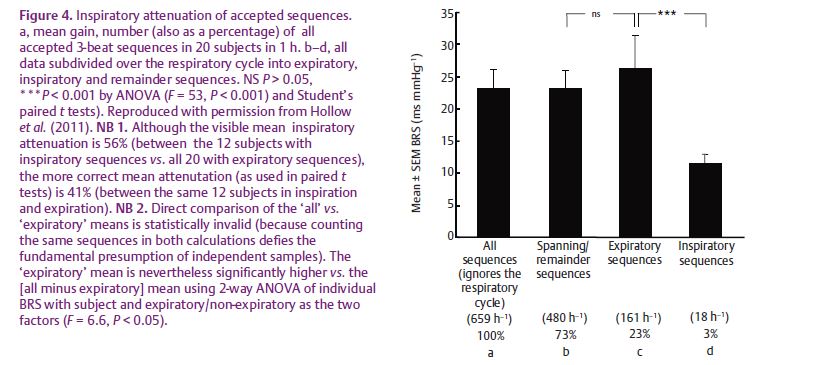
Fourth, if all accepted sequences were random, we would not expect SSA to be able to detect the fundamental properties of the baroreflex, such as inspiratory attenuation. We show (Fig. 4) that SSA does detect inspiratory attenuation. So the small number of random sequences does not prevent SSA from detecting this fundamental property of the baroreflex.
So how good is SSA at measuring baroreflex sensitivity?
The fact that published papers can be selected to show the baroreflex gain value with SSA either agrees or disagrees with those using other techniques is not helpful. This is because we don’t know what is the true baroreflex sensitivity value. The best we can say is that all techniques have advantages and disadvantages. SSA now appears better than previously supposed and appears as good as (and no worse than) any other technique.
Can SSA be improved?
Because of its controversial evolution, numerous fashions have developed in how SSA is carried out, without any being critically evaluated. It is timely to consider whether some standardisation could or should be adopted. For instance, there is no agreement on the minimum time period over which data should be collected, and hence on the minimum number of sequences that should be used to calculate the mean gain value.
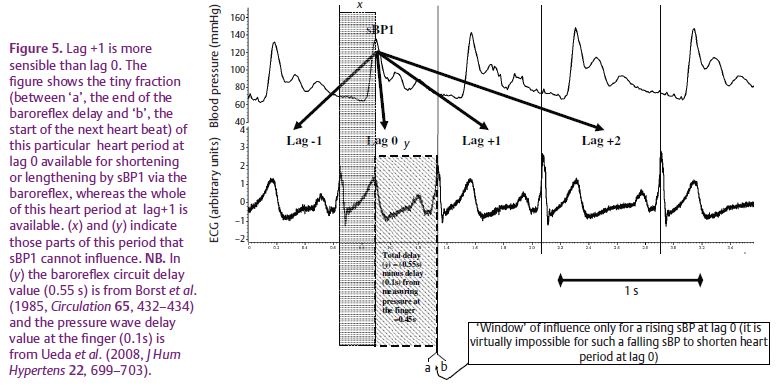
Which lag should be used? Smyth et al. (1969) found that the Oxford technique worked best at lag +1, but SSA studies commonly use heart periods either at lag +1 (the next heart period) or lag 0 (the heart period within which the pressure pulse occurs). Figure 5 shows that lag +1 is more sensible. At lag 0 a falling pressure pulse cannot shorten the early part (x) of the period (unless you believe in time travel!). Furthermore, a low pressure (sBP1) cannot shorten most (y) of the rest of the period because of the finite latency of the baroreflex circuit itself. Thus, falling sequences (~50% of all sequences) can barely shorten heart period at lag 0, whereas rising sequences can still greatly lengthen it. Most SSA studies find no hysteresis (confirming the proposal that hysteresis may depend on the drugs used). SSA studies using lag 0, however, are prone to artefactual hysteresis, because failure to exclude falling sequences will result in accepting ~50% of sequences where it may be physically impossible for low pressure to shorten period.
The effects of breathing could also be taken into account. Failure to exclude attenuated inspiratory sequences reduces the mean baroreflex sensitivity gain value by almost as much as the currently measured effects of ageing, smoking and exercise on baroreflex sensitivity! Alternatively, it might be useful also to measure deliberately the inspiratory attenuation separately, since the vagus nerve in man has negative inotropic as well as negative chronotropic effects on the heart (Lewis et al. 2001) and these may be cardio-protective.
SSA techniques also use a wide variety of data filters before accepting sequences: a minimum filter size of each pressure or heart period change and a minimum filter size of the correlation coefficient (r, or its square, r2) for each slope value. No rationale for such filters has ever been proposed or validated. A number of studies have shown that the r or r2 filter has virtually no effect and, of course, causality cannot be deduced only by correlation. Furthermore, a number of studies have shown that the baroreflex sensitivity gain value depends on which pressure or period filter value is chosen. Yet since we don’t know what the true baroreflex sensitivity gain value is, we don’t know what filter value(s) to choose. It may, therefore, be safer to filter out only pressure changes smaller than the FINAPRES can measure (0.3 mmHg) and smaller than the smallest heart period that can be resolved (e.g.
<1 ms if the ECG is sampled at 2 kHz).
Conclusions
Over 10 years ago John Dickinson (2001) questioned whether we should still continue to measure baroreflex sensitivity. This question still provokes lively debate. Perhaps the final answer will appear when a simple clinical test is devised that predicts hypertension and heart disease sufficiently in advance to enable effective preventative measures to be put in place. Meanwhile, SSA appears a more useful technique for measuring baroreflex sensitivity than previously supposed, as good as (and no worse than) any other baroreflex measuring technique. But there is still scope for its improvement.
References
Dickinson CJ (2001). The baroreflex bandwagon: time to get off? J Hypertens 19, 157–164
Hollow MR. Clutton-Brock TH & Parkes MJ (2011). Can baroreflex measurements with spontaneous sequence analysis be improved by also measuring breathing and by standardization of filtering strategies? Physiol Meas 32, 1193–1212.
Lewis ME, Al Khalidi AH, Bonser RS, Clutton-Brock TH, Morton D, Paterson D, Townend JN & Coote JH (2001). Vagus nerve stimulation decreases left ventricular contractility in vivo in the human and pig heart. J Physiol 534, 547–552.
Mancia G & Mark AL (1983). Arterial baroreflexes in humans. In Handbook of Physiology, Section 2, vol. 3, The Cardiovascular system. Peripheral circulation and organ blood flow, eds. Shepherd JT & Abboud FM, pp. 755–793. American Physiological Society, New York.
Smyth HS Sleight P & Pickering GW (1969). Reflex regulation of arterial pressure during sleep in man. A quantitative method of assessing baroreflex sensitivity. Circ Res 24, 109–121.
