Physiology News Magazine
Microcirculation, metabolic syndrome and exercise
Does exercise dose matter?
Features
Microcirculation, metabolic syndrome and exercise
Does exercise dose matter?
Features
Marcus Vinicius Machado, Ross University School of Veterinary Medicine, Saint Kitts and Nevis
Aline Bomfim Vieira, Ross University School of Veterinary Medicine, Saint Kitts and Nevis
Eduardo Tibiriçá, National Institute of Cardiology, Ministry of Health, Brazil
https://doi.org/10.36866/pn.116.37
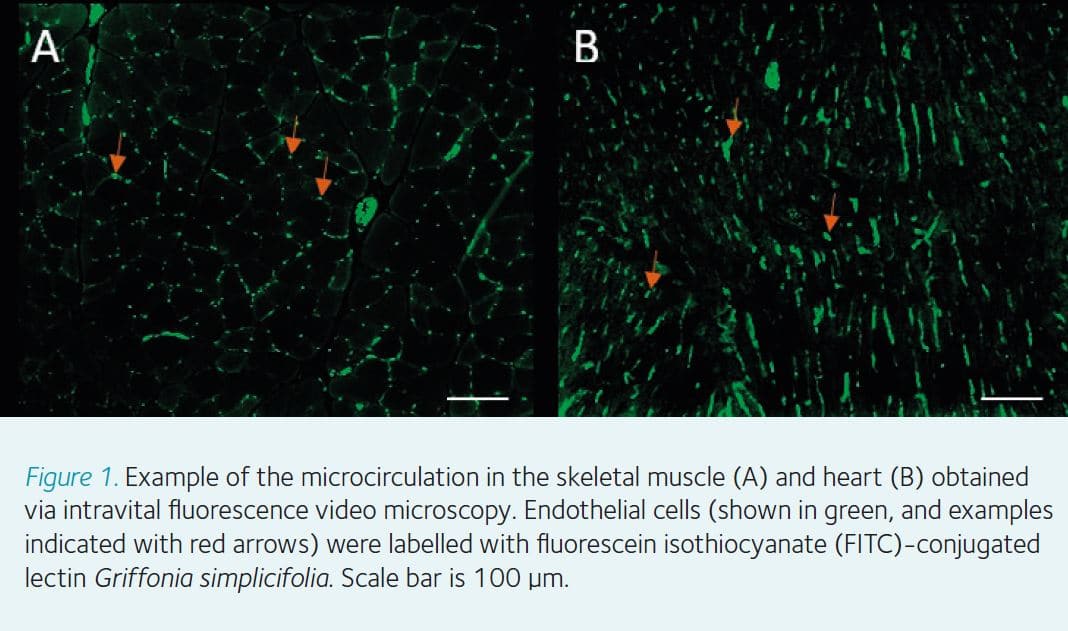
The microcirculation is a branching network of vessels less than 150 µm, only visible through a microscope (Fig.1). This network, composed of arterioles, capillaries, and venules, is primarily responsible for perfusing organs and tissues with blood. Some functions, such as the delivery of oxygen and nutrients and removal of waste products from the tissue, occur almost exclusively in the microcirculation. Because of that, an adequate perfusion via the microcirculatory network is essential for the integrity of tissues and organs. Notwithstanding, abnormalities in microvascular structure and/or function, might contribute to several diseases like myocardial ischemia and stroke.
In recent years, our research group has been dedicated to evaluating the mechanisms and consequences of diseases like hypertension and metabolic syndrome (MS) on the microcirculatory function. MS is the term used to characterise all the risk factors for cardiovascular disease (CVD) that arise from the association of obesity, diabetes mellitus, increased levels of lipids and elevated blood pressure in humans. The association of two or more of these factors significantly increases the likelihood of having damage in organs like the brain, the heart, and the kidneys and consequently increases mortality rates. Here we will provide a brief overview of our data about the dose and benefits of exercise training in the treatment of MS.
How MS impairs microvascular perfusion?
Microvascular rarefaction is broadly defined as a reduction in the number of perfused capillaries in an area of tissue. The rarefaction can be structural, characterised by the absence of capillaries, or functional, in which capillaries are present but they are not perfused. There are currently several pieces of evidence that MS is directly involved with both structural and functional capillary rarefaction in the skeletal muscle, heart and brain (Nascimento et al., 2013; Estato et al., 2017; Machado et al., 2014; Machado et al., 2016).
Although the pathophysiological mechanism involved in microvascular dysfunction during MS is multifactorial and complex, it is widely recognised that the interaction between hyperactivity of the sympathetic nervous system and dysregulation on the release of hormones and pro-inflammatory cytokines is the likely link between the metabolic dysfunctions and microvascular abnormalities (Levy et al., 2008).
The sympathetic nervous system plays a main role in several cardiovascular functions. However, the sympathetic hyperactivity observed both in hypertension and in MS, seems to be an important factor for the microvascular dysfunction and the incidence of CVD. Arterioles are richly innervated by the sympathetic adrenergic fibres and highly responsive to sympathetic vasoconstriction via á1 and á2 adrenergic receptors. Sympathetic system-induced vasoconstriction directly contributes to the functional and structural rarefaction of capillaries, as well as to high blood pressure (Nascimento et al., 2013).
We also investigated some molecular pathways related to the deleterious effects of MS and recently reported increased protein expression of angiotensin-converting enzyme (ACE) and angiotensin II type 1 receptor (AT1R) in an MS model induced by a high-fat diet (Frantz et al., 2017). It is well established that ACE and AT1R can exert deleterious effects on skeletal muscle, such as activation of inflammatory pathways, reactive oxygen species production, and impairment of insulin signalling (Zhou et al., 2015). In addition, ACE activity drives the formation of angiotensin II (ANG II), which stimulates the production of adhesion molecule-1 and macrophage colony in the endothelial wall, increasing vasoconstrictor action and plays a strong atherogenic role (Lyon et al., 2003).
The activation of the inflammatory response through increased expression of proteins involved in the acute-phase reaction and systemic inflammation, such as tumour necrosis factor-alpha (TNF-á) and interleukin 6 (IL-6), increases the expression of adhesion molecules by the vascular endothelial cells and makes their surface adhesive to leukocytes. In the post-capillary venules, increased recruitment of leukocytes may result in capillary obstruction and decreased capillary perfusion. Furthermore, these cytokines stimulate the synthesis of acute-phase proteins by liver hepatocytes (e.g. C-reactive protein [CRP] and fibrinogen), increasing systemic inflammation, platelet aggregation, and plasma viscosity, increasing risk of developing CVD and stroke (Gray and Kim, 2011; Frantz et al., 2017).
Which dose of exercise is beneficial in MS?
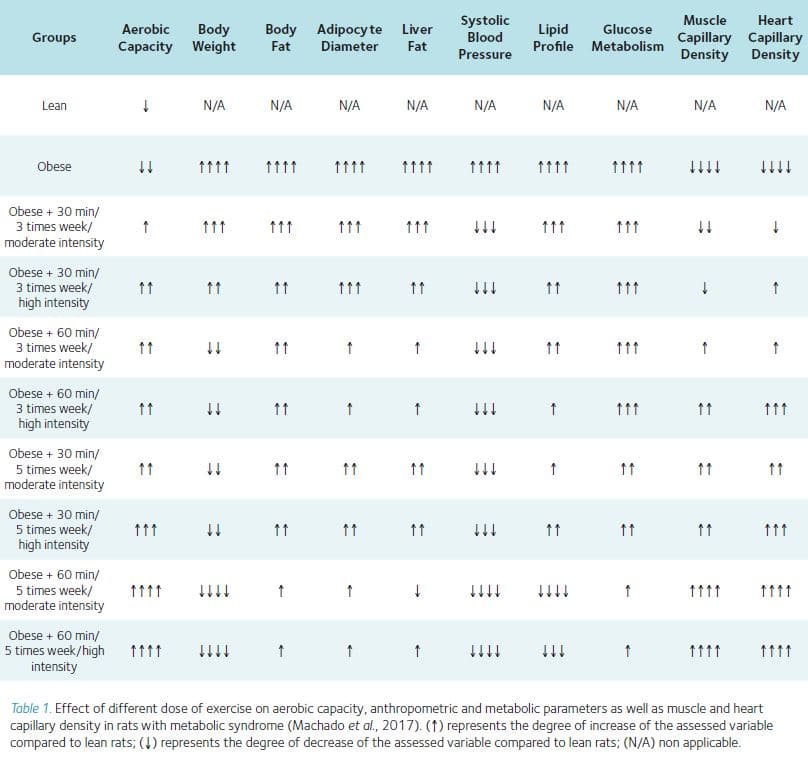
Exercise is one of the most powerful lifestyle interventions to repair the damage caused in the microcirculation by MS. Although there is consensus on the relationship between physical activity and health, the amount of exercise needed to improve several metabolic dysfunctions and reduce the risk of CVD is not clear. In a recently published article “Exercise training dose differentially alters muscle and heart capillary density and metabolic functions in obese rats with metabolic syndrome” (Machado et al., 2017), we provided novel evidence on the adaptive response induced by different combinations of weekly frequency, duration of the session and intensity of exercise effort on metabolic parameters and structural capillary density in rats with MS. A summary of the data on the effects of different combinations of exercise frequency, duration, and intensity on MS parameters and microcirculation is shown in Table 1.
In our study, the animals were fed with a high-fat diet (HFD), and the sedentary group developed obesity, hypertension, diabetes and hepatic steatosis. They also reduced capillary density in the skeletal muscle and heart. On the other hand, even the lowest exercise training dose (30 min/3 times week/moderate intensity) used in this study was able to reduce adipocyte size and the fatty liver (nonalcoholic fatty liver disease – NAFLD).
Interestingly, our results showed that haemodynamic variables (blood pressure and heart rate) were reduced in all animals subjected to exercise regardless of dose. In other words, an increase in frequency, duration or intensity did not provide additional reductions in arterial blood pressure and heart rate in our obese rats.
Regarding glucose metabolism, any exercise dose was able to reduce fasting blood glucose levels, but the glucose intolerance determined by intraperitoneal glucose tolerance test (IGTT) was completely reversed only in the animals who trained five times per week. Therefore, our data showed that an increase in exercise frequency seems to be more advantageous than duration or intensity in reversing insulin resistance (a pre-diabetic state) induced by metabolic syndrome.
Complementarily, we found that exercise frequency (3 or 5 times/week) and duration (30 or 60 minutes) were the main factors improving anthropometric (body weight and body fat) indications, and glucose metabolism (insulin sensitivity and lipid profile) as well as microvascular density in skeletal muscle. The intensity of exercise (high intensity groups) was not the main contributing factor to increased capillary density in skeletal muscle but was nonetheless beneficial to microvascular density in the heart.
In summary, our results demonstrated that exercise frequency and duration are the main factors that improve MS parameters and capillary density in skeletal muscle. The increased intensity was the major factor in reversing microvascular rarefaction in the heart alone. It was noteworthy that while a low dose of the exercise (30 min/3 times week/moderate intensity) was not able to completely reverse the MS dysfunctions, we did observe that this dose was sufficient to normalize blood pressure and attenuate metabolic dysfunctions.
References
Estato V et al. (2017). Cerebral microvascular dysfunction and inflammation are Improved by centrally acting antihypertensive drugs in metabolic syndrome. Metab Syndr Relat Disord 15, 26–35.
Frantz E et al. (2017). High, but not low, exercise volume shifts the balance of renin-angiotensin system toward ACE2/Mas receptor axis in skeletal muscle in obese rats. Am J Physiol Endocrinol Metab 313, E473–E482.
Gray S, Kim JK (2011). New insights into insulin resistance in the diabetic heart. Trends Endocrinol Metab 22, 394–403.
Levy B et al. (2008). Impaired tissue perfusion: a pathology common to hypertension, obesity, and diabetes mellitus. Circulation 118, 968–976.
Lyon C et al. (2003). Minireview: adiposity, inflammation, and atherogenesis. Endocrinology 144, 2195–2200.
Machado M et al. (2014). Physical exercise restores microvascular function in obese rats with metabolic syndrome. Metab Syndr Relat Disord 12, 484–492.
Machado M et al. (2016). Exercise training reverses structural microvascular rarefaction and improves endothelium-dependent microvascular reactivity in rats with diabetes. Metab Syndr Relat Disord 14, 298–304.
Machado M et al. (2017). Exercise training dose differentially alters muscle and heart capillary density and metabolic functions in an obese rat with metabolic syndrome. Exp Physiol 102, 1716–1728.
Nascimento A et al. (2013). Structural and functional microvascular alterations in a rat model of metabolic syndrome induced by a high-fat diet. Obesity (Silver Spring) 21.
Zhou M et al. (2015). Skeletal muscle insulin resistance in salt-sensitive hypertension: role of angiotensin II activation of NFkappaB. Cardiovasc Diabetol 14, 45–53.