Physiology News Magazine
Solidifying my career choice of research – a Rob Clarke Award winner’s account
Membership
Solidifying my career choice of research – a Rob Clarke Award winner’s account
Membership
Klaudia Toczyska
Kings College London,
London, UK
https://doi.org/10.36866/pn.110.42

My undergraduate project was important in shaping my career path. It made me realise how much I enjoy research. I learnt to work independently within the team setting and perform experiments with confidence. I was inspired by my supervisor and members of the group with their motivation and excitement about physiology. Through this experience, I decided to apply for a PhD, and I am currently researching the role of antidepressants in diabetes in the same laboratory. I would recommend that everyone doing an undergraduate degree in science-related subjects should experience a research project to gain useful transferable skills and build a CV.
During my project, I looked at a G-protein coupled receptor’s role in islet development. The endocrine pancreas is made up of small cell clusters called islets of Langerhans, which are composed of three main cell types, α-, β- and δ-cells that produce the hormones glucagon, insulin and somatostatin, respectively. The islet cells act in a co-ordinated manner to maintain plasma glucose levels within a narrow physiological range. Islet β-cells are the only site of insulin production in the body, and insulin is essential for promoting cellular uptake and storage of glucose.
Type 2 diabetes (T2D) develops when peripheral cells do not respond properly to insulin, and β-cell dysfunction means that there is insufficient insulin secretion to compensate for this termed insulin resistance. According to the latest estimations, 425 million adults worldwide have diabetes. There are a number of different drugs approved in the treatment of this metabolic disorder. Therapeutics that increase sensitivity of target organs to insulin (e.g. metformin) or act on β-cells to promote insulin secretion (e.g. sulphonylureas) have been in use for years.
However, with the increasing incidence of T2D comes a requirement to also increase β-cell mass so that insulin secretion can be maintained. G-protein coupled receptors (GPCRs) are popular targets for therapeutic development because many drugs in clinical use target GPCRs and these receptors play an important role in the detection of a variety of signals by β-cells.
G-protein coupled receptor GPR56 hasbeen discovered by my laboratory to be the most abundant GPCR in human islets. In the brain, GPR56 drives cortical development and oligodendrocyte proliferation, but littleis known about its role in the endocrine pancreas.
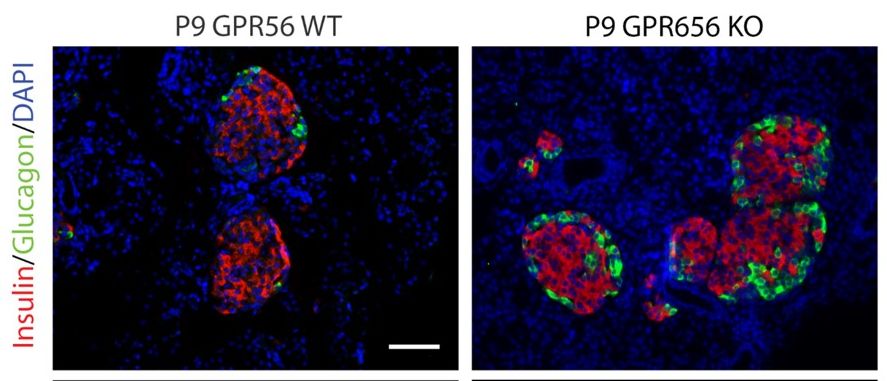
During my undergraduate research project, I worked to determine the role of GPR56 in islet development. Wax and frozen blocks of pancreases from wild-type and GPR56 knockout mice at postnatal day 9 (P9) and mouse embryos at different embryonic days (E11–E18) were sectioned, stained and analysed. I found that GPR56 expression and its co-localisation with transcription factors important in pancreas development (PDX1 and NGN3) were the highest at E15 – the stage of endocrine progenitor cell differentiation into α- or β-cells. At P9, GPR56 was expressed only by β-cells within the islets. GPR56 deletion resulted in a significant decrease in the number of proliferating cells throughout the pancreas at E16 (p<0.05) and E17 (p<0.001). There was also reduced β-cell proliferation in GPR56 knockout pancreases at E16 (p<0.001). These early reductions in proliferation resulted in significant changes in cellular composition of postnatal islets: there was an increased number of α-cells (p<0.01) and decreased number of β-cells (p<0.05) at P9 following GPR56 deletion.
The results of my project show that GPR56 plays an important role in islet development and β-cell proliferation. Therefore, GPR56 could be considered as a candidate drug target in the treatment of T2D, by inducing β-cell proliferation and insulin production sufficient to compensate for insulin resistance.