Physiology News Magazine
Sympathetic nervous system and volume-regulatory hormones: interactions during dehydration
Sympathetic nerve activity and volume-regulating hormones defend blood pressure and blood volume during dehydration. Recent findings showing interactions between these systems give us further insight into the complex adaptations to dehydration.
Features
Sympathetic nervous system and volume-regulatory hormones: interactions during dehydration
Sympathetic nerve activity and volume-regulating hormones defend blood pressure and blood volume during dehydration. Recent findings showing interactions between these systems give us further insight into the complex adaptations to dehydration.
Features
J. A. Rabbitts and N. Charkoudian
Mayo Clinic Rochester, Rochester, MN 55905, USA
https://doi.org/10.36866/pn.81.39

The ability of the human body to adapt to and protect from dehydration has fascinated physiologists for centuries and yet new insight continues to be gained into the mechanisms involved. Further understanding of these interactions has broad implications in healthy populations, from the athlete to the elderly, as well as patient populations, from the acutely dehydrated surgical patient to the acutely or chronically ill medical patient.
Dehydration, along with the associated changes in blood volume and plasma osmolality, elicits a range of physiological responses which must be integrated in order to protect blood pressure and blood volume, thus maintaining perfusion pressure to vital organs such as the brain. In a dehydrated individual, the sympathetic nervous system is activated: increases in cardiac sympathetic activity cause increases in heart rate and stroke volume, while increases in vascular sympathetic activity cause vasoconstriction and maintenance of arterial pressure via increased peripheral resistance. Simultaneously, the renal volume-regulating system is also activated, leading to release of volume-regulating hormones, including angiotensin, aldosterone and vasopressin, which minimize losses in plasma volume via antidiuretic effects on the kidney.
Recently, evidence has emerged that there is an interaction between volume-regulating hormones and the sympathetic nervous system which is not yet fully understood. Many of the volume-regulating hormones have been shown to alter sympathetic neural control mechanisms in several animal models (Fink, 1997; Hasser et al. 2000). For example, Cox and Bishop found that angiotensin administered exogenously to rabbits affects sympathetic nerve activity (Cox & Bishop, 1991). Furthermore, Matsukawa et al. (1991) showed that exogenously administered angiotensin II has sympathetic neural effects in humans.
We were interested in evaluating the influences of endogenous angiotensin in the context of human dehydration. In our first study to address this goal we wanted to know whether the elevation in angiotensin during dehydration is causing neural changes during dehydration in humans. Our hypothesis was that endogenous angiotensin II has a mechanistic role in some of the sympathetic neural changes that are observed in dehydration in normal humans.
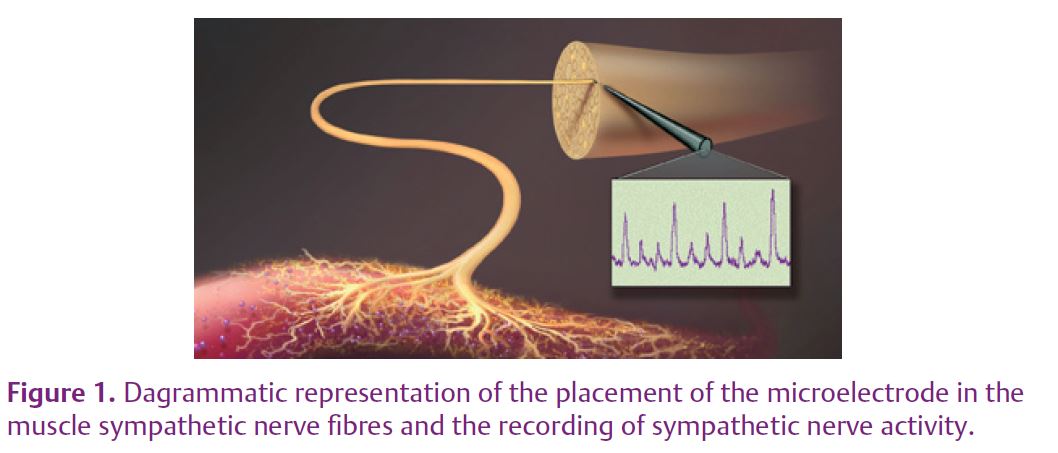
In the lab we are able to measure the electrical activity in sympathetic nerve fibres in humans, specifically postganglionic sympathetic fibres innervating the blood vessels in skeletal muscles (known as muscle sympathetic nerve activity (MSNA)). Although this technique is technically challenging, the data obtained can give unique insight into the beat-to-beat function of the sympathetic nervous system. Figure 1 is a diagrammatic representation of the placement of the microelectrode in the sympathetic nerve fibres and the recording of sympathetic nerve activity. We commonly use the peroneal nerve which is next to the knee and innervates blood vessels of skeletal muscle of the lower leg and foot. Each one of the upward peaks in the MSNA recording is called a burst of sympathetic nerve activity and represents a collection of action potentials in vasoconstrictor nerve fibres. Figure 2 shows actual MSNA recordings in a subject. MSNA is quantified as burst frequency, burst incidence (which controls for difference in heart rates) or total activity (taking into account both burst number and size).
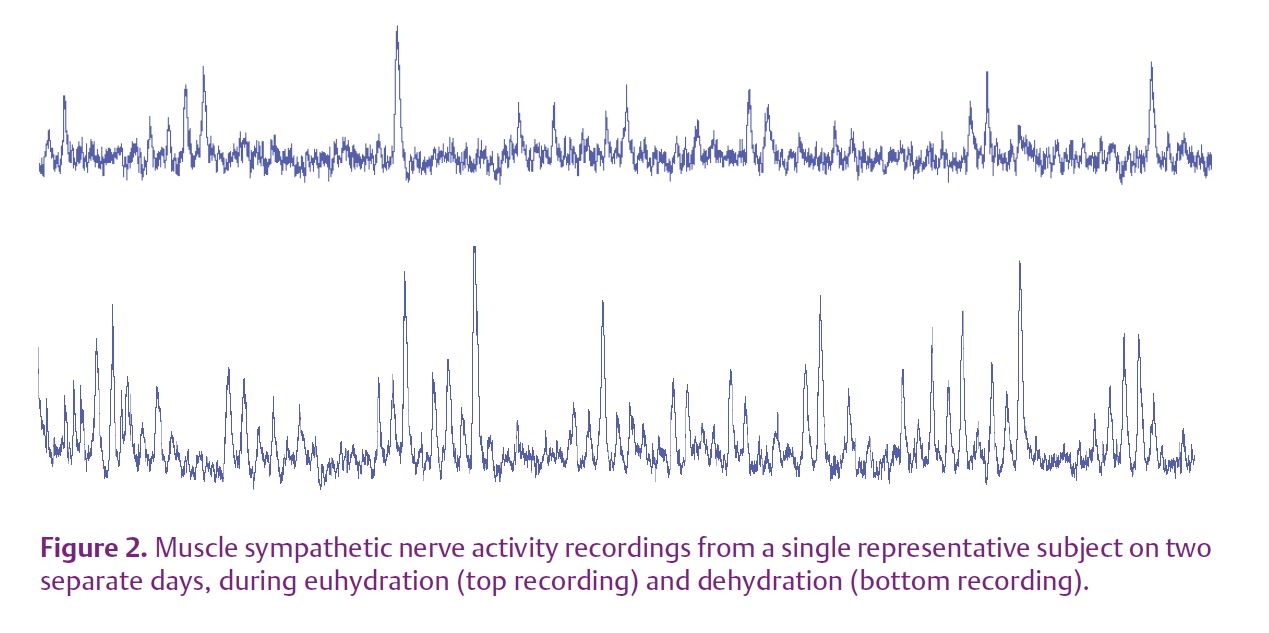
In order to test our hypothesis regarding the role of angiotensin in mediating changes in the sympathetic nervous system during dehydration, we measured MSNA, heart rate and continuous blood pressure in 18 healthy young male and female subjects during euhydration and during dehydration induced by 24 hour fluid restriction (Rabbitts et al. 2009). Figure 2 shows two tracings in the same individual on two different study days, one during euhydration and one during dehydration, illustrating that MSNA is increased during dehydration. With blockade of angiotensin II receptors, this effect was reversed, confirming that in addition to its known volume-regulating effects, angiotensin does mediate some of the sympathetic effects of dehydration. Thus, for the first time in humans we have shown that endogenous angiotensin has sympathetic neural effects which further protect blood pressure during dehydration.
This interaction between the volume-regulating hormones and the sympathetic nervous system to protect blood pressure could have implications in a spectrum of conditions associated with volume depletion and is not yet fully understood. In terms of sympathetic neural effects, the roles of other
endogenous hormones released during dehydration in humans, such as aldosterone and vasopressin, await future study.
References
Cox BF & Bishop VS (1991). Neural and humoral mechanisms of angiotensin-dependent hypertension. Am J Physiol 261, H1284–H1291.
Fink GD (1997). Long-term sympatho-excitatory effect of angiotensin II: a mechanism of spontaneous and renovascular hypertension. Clin Exp Pharmacol Physiol 24, 91–95.
Hasser EM, Cunningham JT, Sullivan MJ, Curtis KS, Blaine EH & Hay M (2000). Area postrema and sympathetic nervous system effects
of vasopressin and angiotensin II. Clin Exp Pharmacol Physiol 27, 432–436.
Matsukawa T, Gotoh E, Minamisawa K, Kihara M, Ueda S, Shionoiri H & Ishii M (1991). Effects of intravenous infusions of angiotensin II on muscle sympathetic nerve activity in humans. Am J Physiol 261, R690–R696.
Rabbitts JA, Strom NA, Sawyer JR, Curry TB, Dietz NM, Roberts SK, Kingsley-Berg SM & Charkoudian N (2009). Influence of endogenous angiotensin II on control of sympathetic nerve activity in human dehydration. J Physiol 587, 5441–5449. http://jp.physoc.org/content/587/22/5441.long