Physiology News Magazine
Vagal baroreflexes in astronauts during spaceflight
Astronauts returning to Earth from space commonly experience orthostatic symptoms, and rarely, frank syncope.
Features
Vagal baroreflexes in astronauts during spaceflight
Astronauts returning to Earth from space commonly experience orthostatic symptoms, and rarely, frank syncope.
Features
Dwain L. Eckberg
Departments of Medicine and Physiology, Hunter Holmes McGuire Department of Veterans Affairs Medical Center and Medical College of Virginia at Virginia Commonwealth University, Richmond, VA, USA
https://doi.org/10.36866/pn.81.32
Astronauts returning to Earth from space commonly experience orthostatic symptoms, and rarely, frank syncope. Since a terrestrial analogue of space exposure, prolonged head-down bed rest, impairs both orthostatic tolerance and vagal baroreflex function, we studied the effects of spaceflight on astronauts’ vagal baroreflexes. We document significant vagal baroreflex impairment in space, which, considered with earlier studies, indicates that exposure to weightlessness diminishes vagal and augments sympathetic cardiovascular influences.

Before the manned space era, scientists expressed trepidation regarding the potentially baleful consequences of human exposure to the totally unknown physiological influences of microgravity. On April 12, 1961, the Soviets launched the first human into space, Yuri Gargarin. He returned to Earth after an 89 min orbital spaceflight with no apparent disability. However, the ninth man in space, the American Wally Schirra, returned after 9 h and 13 min in space and experienced dizziness upon standing up.
Orthostatic symptoms are common in astronauts returning from space; indeed, Buckey et al. (1996) reported that 9 of 14 astronauts could not stand quietly for 10 min, and two of the others felt lightheaded at the end of 10 min. Since a terrestrial analogue of microgravity, prolonged head-down bed rest, provokes both orthostatic hypotension and vagal baroreflex impairment (Convertino et al. 1990), it seemed reasonable to test the hypothesis that microgravity exposure impairs human baroreflex responsiveness.
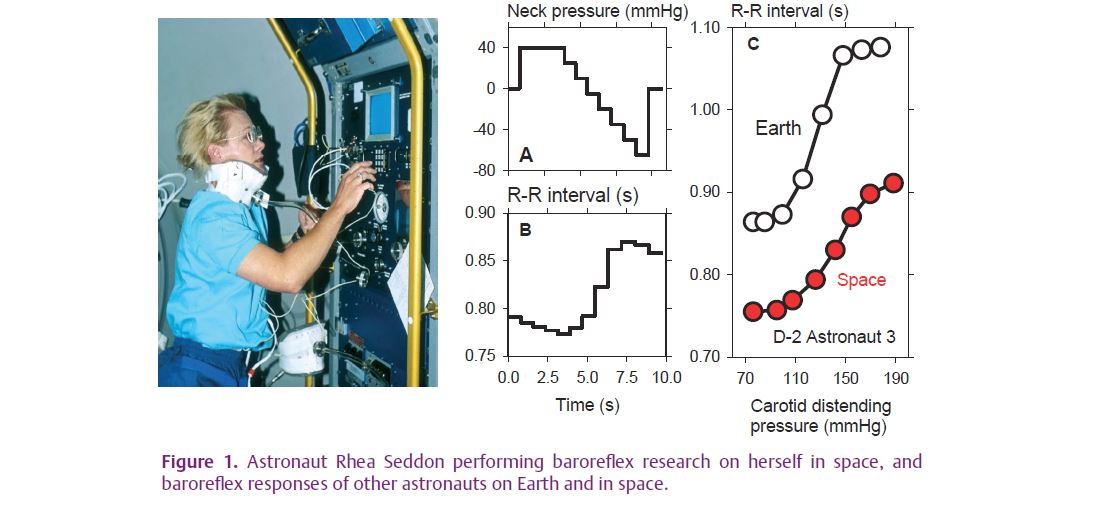
To study this possibility, we modified a neck chamber device (Eckberg & Fritsch, 1993), described originally by British Royal Air Force Flight Lieutenants, J Ernsting and DJ Parry (1957), to elicit entire sigmoidal baroreceptor stimulus–R–R interval response relations during one held expiration. Pressure changes applied non-invasively (and therefore, safely) to the neck provoke parallel linear changes of baroreceptive carotid artery diameter (Kober & Arndt, 1970), which alter vagal and sympathetic neural outflows and trigger baroreflexes responses. Figure 1 shows American astronaut, Rhea Seddon performing baroreflex research on herself in space (left), a stylized neck pressure profile (A), an actual cardiac R–R interval response (B), and responses of a different astronaut before and during spaceflight (C).
We reported responses of 13 healthy astronauts studied before, during and after two space shuttle missions, in a recent issue of The Journal of Physiology (Eckberg et al. 2010). This research was remarkable in the sense that the number of subjects was larger than nearly all studies conducted on astronauts in space. Figure 2 shows mean (±95% confidence intervals) haemodynamic measurements, with data recorded in space shown in red. Systolic, diastolic and pulse pressures varied significantly across days (repeated measures analysis of variance). Diastolic pressure was significantly higher on landing day than on all other study days (Holm–Sidak test); pulse pressure on landing day was significant lower than on flight day 5, and pulse pressure on postflight day 4 was significantly higher than preflight, landing day and postflight day 1; and mean R–R intervals were significantly lower on flight day 8 than preflight.
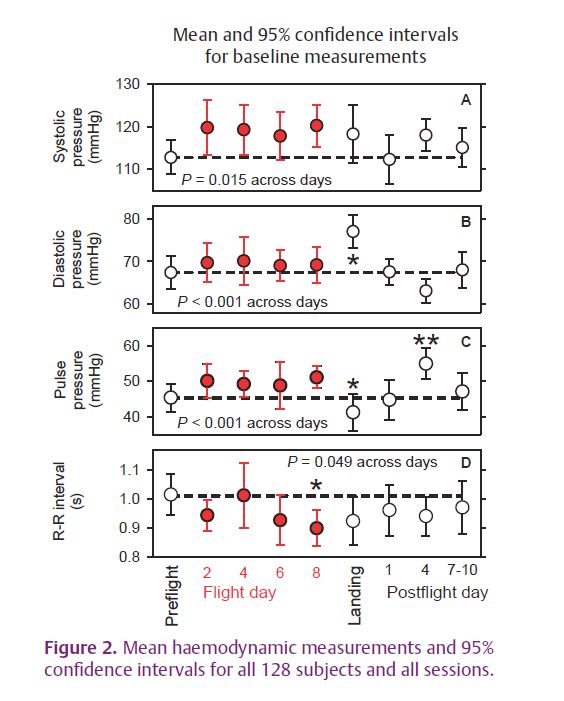
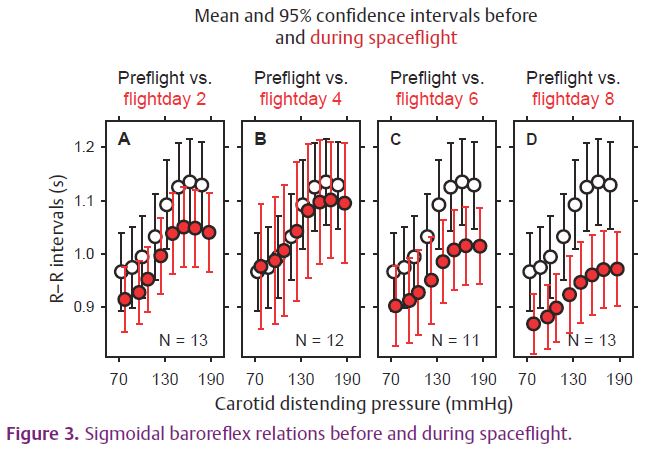
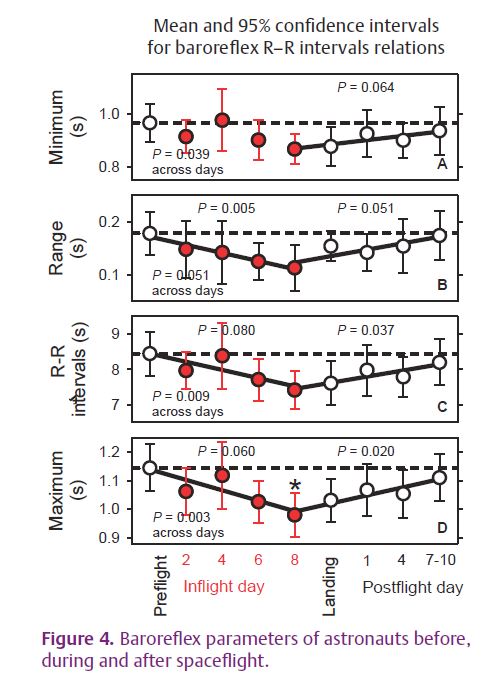
Figure 3 shows mean and 95% confidence intervals of baroreflex stimulus–sinus node response relations for all astronauts before and during spaceflight. With the exception of flight day 4, all average relations were lower in space than during preflight measurements. Ninety-five per cent confidence intervals at higher carotid distending pressures did not overlap by flight day 8. Figure 4 shows changes of individual parameters of sigmoidal vagal baroreflex relations for all sessions. In general, all measurements declined steadily as the space mission wore on, and returned towards preflight levels after astronauts returned to Earth.
Our study fleshes out changes of baroreflex function in space and extends earlier research (Cox et al. 2002), in which sympathetic and vagal baroreflex responses were elicited during spaceflight with Valsalva’s manoeuvre. These results, with those of another study of astronauts (Ertl et al. 2002), suggest that although humans function very well, exposure to microgravity leads to reduced vagal and augmented sympathetic influences in space. Microgravity exposure reduces blood volume, atrophies anti-gravity muscles and impairs vestibular function. Progressive impairment of vagal baroreflex function may represent neuroplastic changes occurring in response to major changes of the autonomic milieu in space. As such, these results may provide a unique perspective on short-lived degradation and subsequent restoration of clinically important human baroreflex function.
References
Buckey JC Jr, Lane LD, Levine BD, Watenpaugh DE, Wright SJ, Moore WE, Gaffney FA & Blomqvist CG (1996). Orthostatic intolerance after spaceflight. J Appl Physiol 81, 7–18.
Convertino VA, Doerr DF, Eckberg DL, Fritsch JM & Vernikos-Danellis J (1990). Head-down bed rest impairs vagal baroreflex responses and provokes orthostatic hypotension. J Appl Physiol 68, 1458–1464.
Cox JF, Tahvanainen KUO, Kuusela TA, Levine BD, Cooke WH, Iwase S, Saito M, Sugiyama Y, Ertl AC, Biaggioni I, Diedrich A, Robertson RM, Zuckerman JH, Lane LD, Ray CA, White RJ, Pawelczyk JA, Buckey JC Jr, Baisch FJ, Blomqvist CG, Robertson D & Eckberg DL (2002). Influence of microgravity on astronauts’ sympathetic and vagal responses to Valsalva’s manoeuvre. J Physiol 538, 309–320.
Eckberg DL & Fritsch JM (1993). How should human baroreflexes be tested? News Physiol Sci 8, 7–12.
Eckberg DL, Halliwill JR, Beightol LA, Brown TE, Taylor JA & Goble R (2010). Human vagal baroreflex mechanisms in space. J Physiol 588, 1129–1138.http://jp.physoc.org/content/588/7/1129.long
Ernsting J & Parry DJ (1957). Some observations on the effects of stimulating the stretch receptors in the carotid artery of man. J Physiol 137, 45P–46P.
Ertl AC, Diedrich A, Biaggioni I, Levine BD, Robertson RM, Cox JF, Zuckerman JH, Pawelczyk JA, Ray CA, Buckey JC Jr, Lane LD, Shiavi R, Gaffney FA, Costa F, Holt C, Blomqvist CG, Eckberg DL, Baisch FJ & Robertson D (2002). Human muscle sympathetic nerve activity and plasma noradrenaline kinetics in space. J Physiol 538, 321–329.
Kober G & Arndt JO (1970). Die Druck-Durchmesser-Beziehung der A. carotis communis des wachen Menschen. Pflugers Arch 314, 27–39.