Introduction
Arm weakness is the most common impairment affecting the quality of life in stroke survivors [1]. Current clinical interventions do not improve outcomes, and gold-standard motion capture methods for motion analysis are costly and require expertise for setup and analysis, limiting their use in clinical settings. Markerless motion capture (MMC), derived through smartphone and/or tablet cameras and AI pose estimation models, could be a promising, accessible alternative to marker-based systems. However, its accuracy for quantifying upper limb movements commonly assessed in stroke rehabilitation remains unclear.
Aims
We therefore aim to initially investigate the accuracy of MMC for common upper limb assessments in non-hemiplegic upper limbs, before evaluating the performance of the method in affected arms.
Methods
Movement data during a simple functional task of drinking from a cup [2] were recorded concurrently using a gold-standard eight-camera marker-based capture (MBC) system (Vicon, recording at 120 Hz) and two RealSense D435 RGB-depth cameras (30 Hz). MMC data were derived from RGB footage from the RealSense cameras by employing a pose estimation model, RTMPose [3], to extract 2D keypoints, which were then triangulated across camera views to produce 3D coordinates [4].
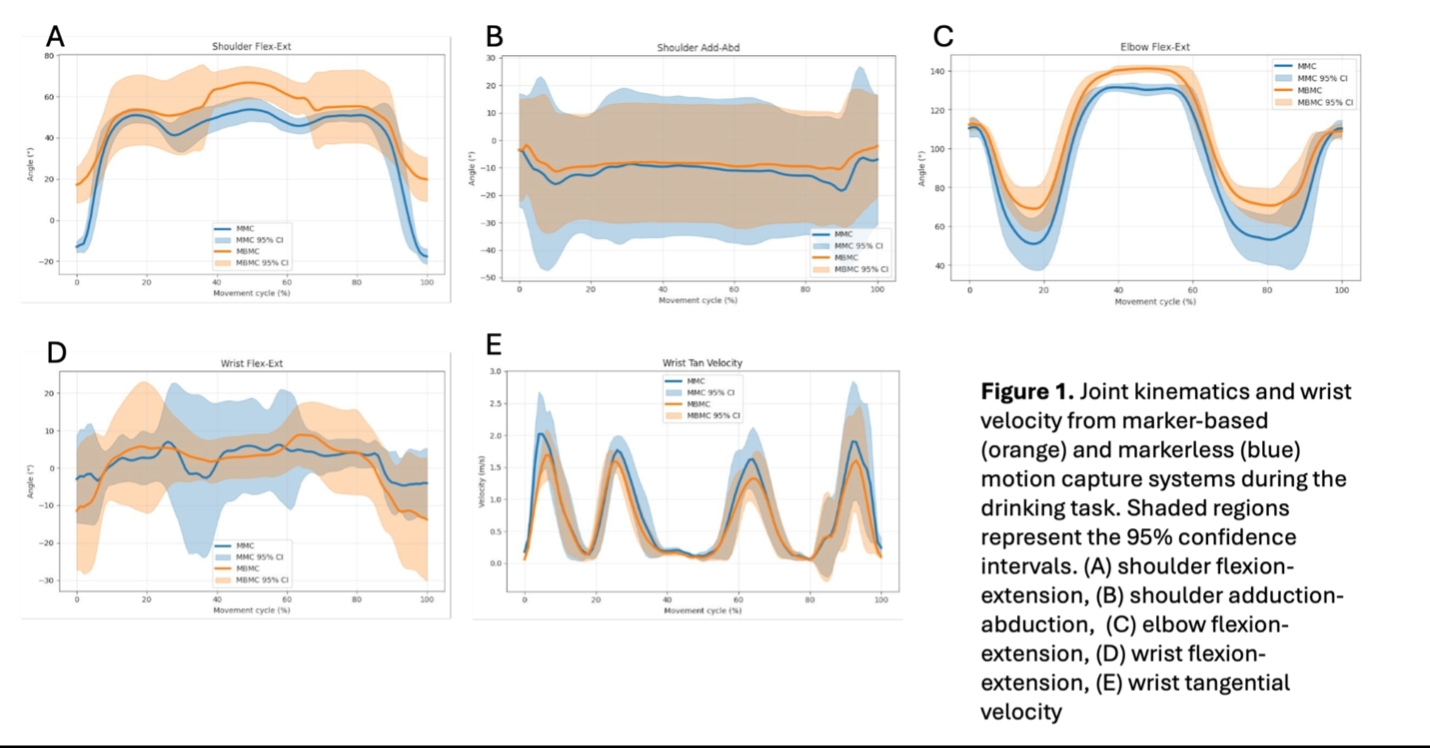
To establish the accuracy of the MMC system, marker-based data were downsampled to allow data overlay (Fig 1A–E). For each joint movement, the Mean Absolute Error (MAE) for the data aggregate and the Coefficient of Multiple Correlation (CMC) for within-subject agreement were calculated.
Results
The MAE of joint angles and tangential velocity (Figure 1 A-E) between the MMC and MBC systems (n = 4, age: 65.25 ± 6.18 years) when performing the drinking task were measured at key joints and movemnts of teh upper lim (Shoulder flexion-extension MAE=16.08°, 95%CI=4.46; Shoulder adduction-abduction MAE=5.92°, 95% CI=2.43; Elbow flexion-extension MAE=12.23°, 95% CI=6.63; Wrist flexion-extension MAE=9.49°, 95% CI=0.86; Wrist TV MAE=0.16 m/s, 95% CI=0.04). Overall the agreement was good for joint ranges and excellent for tangential velocity.
Intra-individual variability was extremely low between the systems for all movements (Shoulder flexion-extension CMC=0.88, SD=0.05; Shoulder adduction-abduction CMC=0.80, SD=0.08; Elbow flexion-extension CMC=0.97, SD=0.03; Wrist flexion-extension CMC=0.80, SD=0.09; Wrist TV CMC=0.98, SD=0.01; Elbow TV CMC=0.97, SD=0.03). These results demonstrate very good to excellent agreement between the systems.
Discussion and Conclusion
Overall, MMC kinematic measures demonstrated good to excellent agreement with MBC data. However, an offset for the starting position was evident between the systems for shoulder flexion joint angles, and greater variability in wrist movements was noted for MMC. Occlusion, as well as concurrent trunk movements, are likely to contribute to these discrepancies and should be explored with a larger dataset.
Nevertheless, the current findings suggest that MMC can be a promising tool to measure outcome measures of arm impairment after stroke. Future work will investigate the system’s ability to accurately measure arm movement in the affected upper limbs of stroke survivors.
Ethical consideration:
The research project has been approved by teh King’s College London Research Ethical Committee.