Physiology News Magazine
Applied physiology in the COVID-19 pandemic:
Measurements on the frontline
Membership
Applied physiology in the COVID-19 pandemic:
Measurements on the frontline
Membership
Brendan Cooper, President, Academy for Healthcare Science, University Hospitals Birmingham NHS Foundation Trust
https://doi.org/10.36866/pn.121.40
Within the National Health Service (NHS), clinical physiologists contribute an enormous amount to routine clinical services and are based both in out-patient and in-patient roles. There are at least eleven professions in physiology delivering a wide range of physiological techniques: audiology, autonomic neurovascular function, cardiac physiology, clinical perfusion science, critical care science, gastrointestinal physiology, neurophysiology, ophthalmic and vision science, respiratory and sleep physiology, urodynamic science and vascular science.
Traditionally, clinical physiologists or scientists performed mainly diagnostics, but in recent decades, roles have evolved into delivering interventions and treatments, often including monitoring, across the spectrum of professional specialisms. These services can take place in venues as diverse as the patient’s home, operating theatres, critical care units and hospital wards. Variety, flexibility, and varied complexity are common themes across all clinical physiology roles.
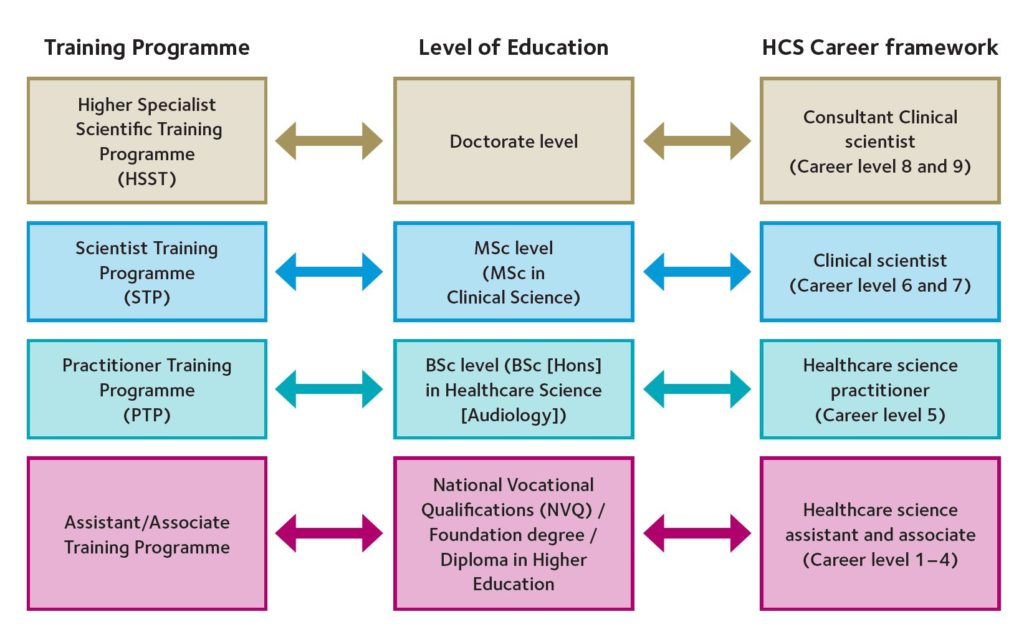
Clinical physiologists generally use techniques that measure pressure, flow, volume, electrophysiological activity, or imaging, to support clinical diagnostics. There are training pathways in most of the professions, which are part of the national training programmes run by the National School for Healthcare Science (NSHCS), or professional body programmes. All training programmes have theoretical and practical components, and courses ensure that practitioners understand not only the physiological principles but achieve clinical competence in appropriate techniques (Fig. 1). Entry level for graduates at Bachelor’s, Master’s or doctoral level is possible, with the Master’s level Scientific Training programme (STP) being the most popular option for graduates. These training courses are often themed in groups of physiological specialities (e.g. cardiac, respiratory and vascular).
Clinical physiologists and scientists often work directly with patients to measure and monitor particular conditions, using their knowledge and competencies in physiological systems, such as:
- Carrying out echocardiograms to check how the heart is working;
- Undertaking diagnostic tests of flow, pressure, and volume to assess lung function;
- Measuring eye function and taking images of the eye and its supporting structures;
- Assessing hearing and balance function in everyone from babies to the elderly;
- Investigating the nervous system to diagnose and monitor things like epilepsy and multiple sclerosis;
- Diagnosing and treating patients with sleep problems such as sleep apnoea, where people temporarily stop breathing.
Clinical physiologists are very much applied physiologists, and it is interesting to examine a typical diagnostic test that incorporates the applied physiology that is essential on the frontline of the NHS. In respiratory and cardiac physiology, the cardiopulmonary exercise test (CPET) is regarded as the “gold standard” to evaluate the limitations of physiological performance of the body in health and disease. One reason for this is that the physiological and metabolic stress of surgery is related directly to the ability to perform beyond a threshold of exercise ability. Indeed, patients who fail (so to speak) such pre-operative CPET tests often require more critical care and have higher mortality than those who pass the threshold.
CPET essentially requires the subject to breathe through a flow-measuring device (e.g. pneumotachometer, ultrasonic flowmeter, hot-wire anemometer, mass flow meter) and the signal is integrated to produce volume as well as measuring respiratory rate. From these signals, minute ventilation, tidal volume, and other subdivisions of volumes and capacities are calculated. Expired gas analysis using oxygen cells and infrared gas analysers, together with the volume signal, calculate oxygen uptake, carbon dioxide production and other calculated values from these. In addition, the electrocardiogram is used to monitor the electrophysiology of the heart, but also to calculate heart rate and oxygen pulse, which is an estimate of stroke volume utilising rearrangement of the Fick equation (CO = VO2/(Ca – Cv). This is classic physiology utilised in direct patient measurement!
Pulse oximetry is essential to monitor oxygen trends during the test, and quite often an arterial or “arterialised” blood gas can be used to measure blood-gas status and derive the ratio of dead-space to tidal volume (VD/VT) or the alveolar–arterial difference as an assessment of gas exchange.
Of course, all these physiological methods require calibration of equipment, validation of signal quality and are usually part of an overall quality control scheme in physiology departments. In recent years accreditation of NHS physiological services has meant that several centres now have UK Accreditation Service (UKAS) compliance as part of the scheme called Improving Quality in Physiological Service (IQIPS). This means that patients are protected by not just safe measurement, but safe and reliable processes from their appointment to the final report.
There are many other examples of the use of applied physiology in any of the physiological professions listed above. For physiology graduates, a career as a physiologist in the NHS is not just rewarding, but one of the most interesting and varied careers for scientists in the NHS (in my biased opinion, of course!). This has been exemplified recently by the deployment of physiologists to support the front line of the COVID-19 pandemic.
The COVID-19 pandemic has changed the role of healthcare physiologists and their standing within hospitals and healthcare across the UK in an unimaginable way. Whilst many of the routine services delivered daily have scaled back, clinical physiologists have been on wards and in critical care delivering their usual essential services, often in full PPE, but under very stressful situations. Furthermore, because of their clinical skills with meeting, handling and caring for patients, they have also been deployed to support on wards acting sometimes in a healthcare assistant role – taking regular observations (temperature, blood pressure breathing and heart rates), assisting with patient direct care (bedpans/commodes!) and talking with patients who are often scared, lonely and anxious. This utilises the “care” part of being a healthcare scientist and makes the role more fulfilling, as well as occasionally exhausting.
Respiratory physiologists have been used on COVID-19 wards to support continuous positive airways pressure (CPAP) and high flow nasal oxygen (HFNO) in some very sick patients, often working overnight, at weekends and/or long shifts. Ventilators are often used clinically in accordance with clinically agreed protocols, but having an understanding of the underlying physiology – lung compliance, airflow, gas exchange, response times, physiological variation, all contribute to gaining confidence and understanding at the bedside. Sometimes you may have the opportunity to teach nurses or junior doctors about the physiology of the ventilation, the physiology of coronavirus or the reasons why a particular probe is not working.
Many physiologists (from all professions including audiology, neurophysiology, GI physiology etc.) and at different grades from juniors to consultant clinical scientist level, have been redeployed to support critical care teams looking after intubated, ventilated patients. Others have assisted with infection protection and control by ensuring all clinical staff going on to wards or ITU use the correct personal protective equipment (PPE) procedures during “donning and doffing” of protective equipment. Scientists are very good at quickly retraining and adopting new roles in a controlled and consistent manner – perhaps something learnt in the methodical scientific approach to their work on a daily basis. No task is too menial in this COVID-19 emergency.
I hope there are some physiology graduates and postgraduates reading this, who feel they may want to work in a more clinical patient-facing role, or even expand their research from the bench to the bedside, and may be inspired to become clinical physiologists or scientists. There are often many vacancies and sometimes niche ways of joining the profession as well as coming through the training programmes listed above. Often hospitals will offer in-service training programmes or apprenticeships for graduates (e.g. sports science graduates often get trained in respiratory and cardiac physiology departments).
To study physiology and then spend your career delivering applied physiology and conducting physiological research is an enormous privilege. And to be on the frontline of the NHS during this pandemic and help patients is an absolute honour!
Further reading
National School of Healthcare Science https://nshcs.hee.nhs.uk/
Academy for Healthcare Science https://www.ahcs.ac.uk/
Four Nations’ Chief Scientific Officer Offices:
England https://www.england.nhs.uk/ healthcare-science/cso-programmes/
Wales https://gov.wales/dr-rob-orford
Scotland https://www.gov.scot/ policies/health-workforce/ healthcare-scientists/
Northern Ireland https://www.nidirect. gov.uk/articles/healthcare-scientist