Physiology News Magazine
Editorial: Physiology on the frontline
News and Views
Editorial: Physiology on the frontline
News and Views
Julia Turan, Managing Editor, Physiology News
Keith Siew, Scientific Editor, Physiology News
https://doi.org/10.36866/pn.121.4
Little did we know, when we chose to dedicate an issue to this theme back in early January 2020, that it would land at a time so apropos. Now, as we sit here writing this editorial, over a year later and approaching the end of our third national lockdown, we must admit that this issue has been more challenging than most to assemble, as colleagues were redeployed to rapidly filling wards or scrambling to restructure their teaching at a moment’s notice. So, it is with sincerest thanks to our contributors and great excitement that we welcome our readers to this Special Issue of Physiology News focusing on the interplay between physiology and medical technology in patient care (something of which we are all more acutely aware of late).
Today, with the plethora of devices beeping, humming and buzzing about a modern hospital ward, it is perhaps easy to forget that the practice of extending our senses to explore physiological phenomena is centuries old. Some of the earliest of these devices can be dated back to the beginning of the 17th century, at a time when a patient’s pulse rate was calculated not by time but length using a pulsilogium. Invented in 1602 by Santorio Santorio, the pulsilogium took advantage of his friend’s insight (incidentally Galileo Galilei) into the frequency of a pendulum’s oscillation being inversely proportional to the square root of its length. And so, by synchronising the swing of a pendulum to a patient’s pulse through adjustment of the cord length as measured against a ruler, heart rate could be accurately determined for the first time (Fig. 1, left). In 1612 he went on to describe the thermoscope, another creation by his friend Galileo that he repurposed for medical usage. Composed of an air-filled glass ball attached to a long, thin graduated glass pipe submerged in a reservoir of water (Fig. 1, right), he could measure (semi-quantitative) changes in a patient’s temperature as a column of water moved up/down the glass pipe upon placement of the glass ball in either the hand or mouth. These, combined with his “weighing chair” invention, were the first truly quantitative tools for physiological experiments and his pioneering of their clinical usage forever changed patient assessment.

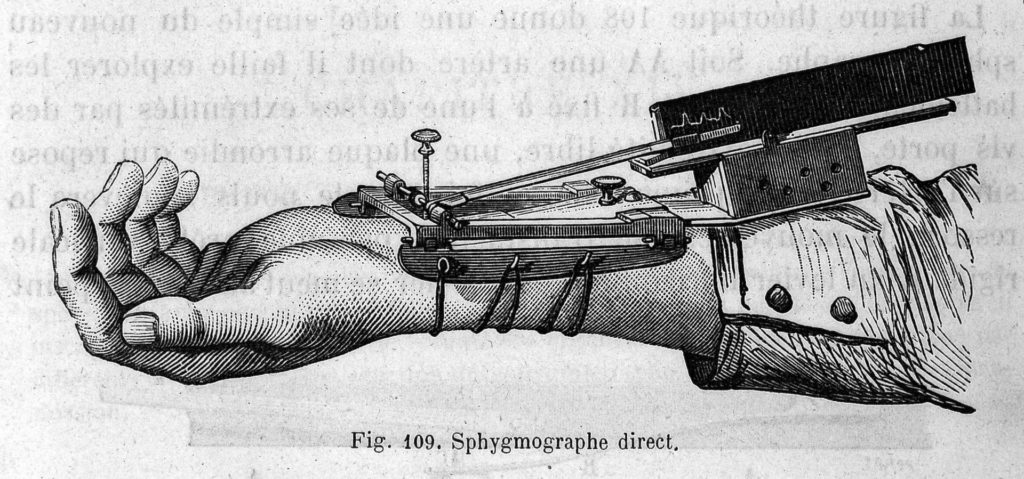
The next advancement in assessing the heart would come with the invention of the stethoscope in 1816 by René Laennec, which came about not through rigorous scientific endeavours but rather because of embarrassment at the seeming impropriety of putting his ear to the chest of a young female patient. Serendipitously, he discovered that a rolled-up tube of paper (later refined into a wooden tube) could augment the auscultation of heart sounds (Fig. 2). Following in the trend of non-invasive measurements, the sphygmograph – a system of levers and weights used to stop blood flow in the radial artery – was developed in 1854 by Karl von Vierordt to estimate blood pressure, and later modified to record pulse waves (Fig. 3). These early innovations have paved the way for their 21st century digital descendants, and during this period of social distancing, heart-monitoring smartwatches have been used to detect life-threatening episodes of atrial fibrillation in outpatients (p. 14).

It is also easy to forget that the practice of medicine is not confined to bipedal hominids, but also extends to our furry companions and the progress made in veterinary care and animal experimentation often precedes human care (p. 10). None better encapsulates this than Augustus Desiré Waller who toured the lecture circuit with his dog Jimmy, demonstrating the utility of his recently (c.1887) invented electrocardiogram. In 1913, Abel, Rowntree and Turner demonstrated the first use of an “artificial kidney” in living animals, an essential milestone in the development of the modern dialysis devices keeping millions alive today (p. 26). And in a more modern example, Hagisawa et al. (p. 22) have shown the utility of their novel artificial blood products in haemorrhagic emergencies in the veterinary setting, and have now commenced their first clinical trials for human use.
However, perhaps the best example of the convergence of medical technologies and physiology have centred around this pandemic. Indeed, many physiologists have and continue to play significant roles in the COVID-19 response. In particular, the work of the Doyle group (p. 19), who specialise in the treatment of thrombi, will be of increasing importance in understanding the pathophysiology of COVID-induced thromboembolism (with overall rates of venous thrombosis averaging 21% among non-ICU hospitalised patients). The issue also includes perfusionists sharing their experiences of providing ECMO life support to the most critical patients (p. 38), and an account of the redeployment of physiologists ranging from audiology, neurophysiology and gastrointestinal physiology to support critical care teams and patients (p. 40).
And we hope you too are as amazed as us by the work of our clinical physiologist colleagues.