Physiology News Magazine
Ventilating the furry ICU patient:
A veterinary perspective on mechanical ventilation in the ICU
Features
Ventilating the furry ICU patient:
A veterinary perspective on mechanical ventilation in the ICU
Features
Helen Wilson, Langford Vets, University of Bristol, UK
https://doi.org/10.36866/pn.121.10
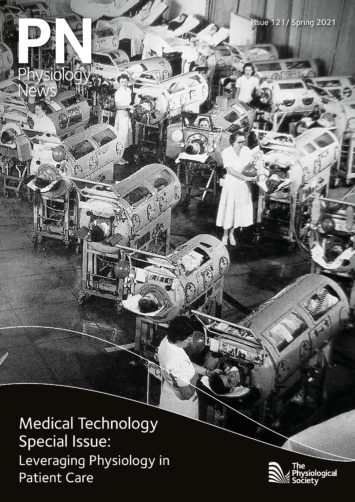
Modern mechanical ventilators are a far cry from their “iron lung” predecessors and yet, in this COVID-19 pandemic, we have intensive care units filled with rows of patients on ventilators, just as we did in the 1950s, with rows of poliomyelitis patients confined to the metal cylinders that were their only means of breath. The COVID-19 pandemic has put the indispensable mechanical ventilator firmly into the public arena once more.
Modern permutations of ventilators are highly complex pieces of equipment capable of monitoring tidal volumes and airway pressures, as well as responding to patient respiratory efforts. They even come complete with disco-esque flashing lights and musical alarms (which I often hear in my sleep). Mechanical ventilation is employed not only for humans, but also to help our furry companions breathe more easily, which came full-circle last year when the ventilators from our veterinary hospitals were re-deployed to human hospitals to help meet the demand at the start of the pandemic.
Poliomyelitis epidemics were frequent throughout the first half of the 20th century, with 1 in 200 victims suffering respiratory paralysis and requiring ventilatory support via an iron lung. Patients often had secondary pneumonia and survival rates were poor, around 15 – 20% (Woollam, 1976).
The iron lung worked on the principle of negative pressure ventilation. It was essentially a sealed chamber containing the patient’s body, with only their head protruding. A pump generated a sub-atmospheric pressure within the chamber, which consequently expanded the patient’s rib cage, thus increasing the intrathoracic volume and in turn generating negative pressure within the thoracic cavity, to draw air into the lungs through the nose and mouth.
In Copenhagen in 1952, Drs Henry Lassen and Bjørn Ibsen developed the technique of providing manual intermittent positive pressure ventilation through a high tracheostomy for poliomyelitis patients, and saw a dramatic reduction in their mortality figures from 80% to 40% (Woollam, 1976). Cue the era of the modern mechanical ventilator.
Despite the better success rates of positive pressure ventilation, there are a number of physiological advantages of negative pressure ventilation. A normal physiological inspiration is a negative-pressure event, generated by the contraction of the external intercostal muscles and the diaphragm, expanding the thoracic cavity and reducing the intrathoracic pressure, thus drawing air into the lungs, in exactly the same way as the iron lung. A positive pressure breath is essentially the opposite of a physiological breath. Air is forced into the lungs at supra-atmospheric pressure, to forcibly expand the pulmonary parenchyma. With both types of ventilation, expiration is passive, relying on the elastic recoil of the chest as in normal resting expiration. Intuitively, it makes sense to use negative pressure over positive pressure ventilation for its greater alignment with normal physiology, but both modalities have limitations. Modern medicine focuses on positive pressure ventilation, due to its superior control over pulmonary dynamics and advantages for ventilating diseased lungs.

Initiating positive pressure ventilation in dogs and cats
The aim of mechanical ventilation is to maintain normal oxygenation and ventilation, with the least aggressive ventilator settings. In veterinary critical care, there are three criteria for initiating mechanical ventilation, of which a patient need fulfil only one (Vassilev and McMichael, 2004). First, severe refractory hypoxaemia; second, severe hypoventilation; and third, excessive work of breathing with impending respiratory fatigue or failure. Hypoxaemia is defined as partial pressure of arterial oxygen (PaO2) < 80 mmHg and hypoventilation as partial pressure of arterial carbon dioxide (PaCO2) > 45 mmHg. In veterinary medicine we use the 60/60 rule for determining the need for mechanical ventilation. If the PaO2 is < 60 mmHg, or the percutaneous oxygen saturation (SpO2) is < 90% as an equivalent marker of oxygenation, despite oxygen therapy, or if the PaCO2 is > 60 mmHg despite treatment, then mechanical ventilation is indicated. The third criterion is a clinical decision and allows for the institution of mechanical ventilation if a patient’s welfare is severely compromised by their dyspnoea.
There are five causes of hypoxaemia (West, 2008):
- Hypoventilation
- Ventilation–perfusion (V/Q) mismatch
- Right-to-left shunt
- Diffusion impairment
- Reduced oxygen tension in inspired air (PiO2), i.e. hypobaric or inspiratory hypoxia
Total oxygen content in the blood is further affected by anaemia and aberrant haemoglobin species, but these patients will have a normal PaO2 and therefore will not benefit from mechanical ventilation; rather they require restoration of their haemoglobin levels to improve their tissue oxygenation.
Hypoventilation results in reduced minute volume and inadequate elimination of CO2 from the lungs, hence these patients develop hypercarbia (i.e. increased blood CO2). Hypoventilation is always associated with hypoxaemia, due to a failure of fresh gas delivery to the alveoli, but the hypoxaemia is readily reversed with oxygen supplementation, while the PaCO2 remains unchanged without mechanical ventilation.
Ventilation–perfusion (V/Q) mismatch and shunt are a continuum of disease severity and are the most common reasons for hypoxaemia to occur in veterinary medicine. For oxygen to diffuse into the blood and for carbon dioxide to diffuse out of the blood, there must be even matching of the alveoli that are being ventilated (receiving air) and those that are being perfused. If ventilation and perfusion were perfectly matched across the lungs, the V/Q ratio would be 1 (Fig. 1A).
V/Q matching is not perfect in healthy lungs, resulting in a V/Q ratio of 0.8 averaged across the whole lung, because of the effect of gravity on the distribution of perfusion from the top to the bottom of the lungs and the effect of the weight of the lungs on ventilation. that which are being ventilated but inadequately perfused are called high V/Q units (Fig. 1B) and those being perfused but inadequately ventilated are low V/Q units (Fig. 1C).
Zero V/Q units are alveoli that are being perfused but receiving no ventilation and this indicates alveolar collapse or small airway obstruction. Zero V/Q units give rise to a right-to-left pulmonary shunt, which is a region of lung that is perfused but not ventilated, resulting in blood entering the left side of the heart that has traversed the lungs without picking up any oxygen. This volume of blood is called the shunt fraction.
Hypoxaemia due to zero V/Q units or whole regions of diseased lung resulting in shunt will not respond to oxygen supplementation and requires positive pressure ventilation to open up these collapsed alveoli. It is unlikely that negative pressure ventilation would be helpful for such severely compromised regions of lung. We often perform so-called recruitment manoeuvres on ventilator patients to transiently increase the pressure within the airways and open up collapsed regions of alveoli in severely diseased lungs, thus improving V/Q matching.
Diffusion impairment results in hypoxaemia through thickening of the barrier between the alveolar and capillary lumens. This can occur in pulmonary fibrosis, which can develop secondary to severe inflammatory diseases such as acute respiratory distress syndrome (ARDS). ARDS can result from many diseases, including SARS-CoV-2 infection (COVID-19) and it remains to be seen if people who have recovered from COVID-19 will go on to develop pulmonary fibrosis and longer-term hypoxaemia. Because carbon dioxide has greater solubility than oxygen, it diffuses 20 times faster, meaning that hypercarbia is rarely due to diffusion impairment, whereas hypoxaemia can be.
Finally, hypoxaemia can be due to reduced fraction of inspired oxygen (FiO2), typically due to equipment failure when animals are intubated and connected to a breathing circuit.
Assessing ventilation and oxygenation in animals
Hypoventilation can be easily assessed on a venous blood gas sample, due to the consistent difference of 3 – 6 mmHg between arterial and venous PCO2 in animals (Lumb, 2017). Conversely, assessing oxygenation can be challenging in veterinary medicine. Minimal handling is important for dyspnoeic patients, particularly cats, as they are prone to cardiopulmonary arrest when stressed. This can make obtaining an arterial blood gas challenging. Pulse oximetry can provide us with a surrogate marker of oxygenation but is also fraught with difficulty. Sadly, we cannot ask our patients to sit still while we put a probe on their finger. Our patients’ fur also interferes with pulse oximetry readings. The most reliable place to obtain a pulse oximeter reading from is the tongue, which is only feasible when the patient is under anaesthesia if you value your fingers and the probe. The buccal mucosal membrane is the best place to obtain a reading from in a conscious patient (Fig. 2) but is frequently pigmented in animals and often poorly tolerated, resulting in unreliable readings. Alternative mucous membranes that can be helpful include the prepuce and vulva and less-furry areas that may be fruitful include the inguinal region, ears and digits.

The problem of oxygen toxicity
Interestingly, oxygen itself can be toxic and veterinary species are more susceptible than humans (Lumb, 2017). Oxygen is a free radical, possessing two unpaired electrons. This makes it and some of its derivatives highly reactive, with a tendency to steal electrons from other molecules. Fatty acids in membrane phospholipids are particularly rich in readily available electrons and therefore highly prone to oxidative damage. Free radical oxidative damage to cell membranes triggers apoptosis and inflammation. In the lung, this can lead to hyaline membrane formation and progressive fibrotic change, with histological changes indistinguishable from those associated with ARDS. The toxic threshold is an FiO2 of 50% for 24 hours or more (Fisher et al., 1984). For this reason, we always aim to reduce the FiO2 to below this threshold within the first 24 hours of mechanical ventilation, although this is sometimes not possible due to disease severity.
Ventilating healthy vs. diseased lungs
Patients requiring ventilation fall into one of two groups – those with healthy lungs and those with diseased lungs. Patients with healthy lungs requiring mechanical ventilation are those with neurological diseases causing hypoventilation. Negative pressure ventilation may be effective for patients with healthy lungs but is less likely to work adequately for patients with diseased lungs, particularly those with severe disease and regions of zero V/Q units and shunt. These patients require the application of positive pressure breaths to open up and recruit the collapsed regions of lung to alleviate their hypoxaemia (Brower et al., 2000), thus explaining the mortality benefit over negative pressure ventilation discovered by Drs Lassen and Ibsen in poliomyelitis patients, who frequently had secondary pneumonia.
However, all pulmonary diseases in dogs and cats can result in reduced compliance, meaning that the lungs are stiffer and expand by a smaller volume for any given increase in pressure compared with healthy lungs. Positive pressure can damage the lung, both by excessive pressure (barotrauma) and by excessive volume (volutrauma). Together, these sequelae of positive pressure ventilation are called ventilator-induced lung injury (VILI). VILI can lead to worsening inflammation of the lungs, worsening compliance and even pneumothorax. The risk of VILI is increased as pulmonary compliance worsens and VILI is associated with an increased risk of death in ARDS (Brower et al., 2000). Interestingly, in 1951, Plum and Lukas noted an association in negative pressure ventilation between larger tidal volumes and the development of pulmonary emphysema, implying that excessive negative pressure can also cause a form of VILI.
The importance of prone positioning in ventilated people was recognised as early as 1952 and was a problem of negative pressure ventilators, which did not allow for this (Woollam, 1976). Prone positioning has been shown to reduce mortality in humans with ARDS undergoing positive pressure ventilation (Sud et al., 2014) and recently has been shown to avert 1 in-hospital death for every 8 patients ventilated with ARDS due to COVID-19 (Shelhamer et al., 2020). This is because in the prone position, the volume of lung that is collapsed under its own weight is reduced compared with the supine position, thus improving V/Q matching. Dogs and cats are naturally in the prone position during mechanical ventilation, offering us an advantage compared with our human counterparts (Fig. 3).

Newer respiratory support technologies in the veterinary ICU
The rise of less invasive technologies such as continuous positive airway pressure (CPAP) and high-flow oxygen have helped to reduce the number of patients that require mechanical ventilation and the associated morbidities. When delivered via a mask, CPAP is not well tolerated by veterinary patients without heavy sedation, as animals dislike having a mask over their face and the long noses of dogs do not fit the masks well. Therefore, CPAP can only effectively be delivered to animals via a helmet (Ceccherini et al., 2020) or to intubated patients. There are a number of limitations to helmet ventilation and, consequently, we most commonly use CPAP as a means of weaning patients from mechanical ventilation, rather than a way of negating it. On the other hand, high-flow oxygen is proving extremely useful in the veterinary ICU. High-flow oxygen is warmed, humidified oxygen, which can be delivered through nasal prongs at significantly higher flow rates than traditional oxygen therapy, therefore dramatically improving PaO2 (Jagodich et al., 2020). The humidification means it is much better tolerated and less likely to cause desiccation of the nasal turbinates (the mucosal surfaces within the nasal cavity), which leads to patient discomfort and the risk of rhinitis from secondary infection. In addition, the delivery of high-flow oxygen requires fewer resources and less expertise than mechanical ventilation, making it significantly cheaper. In the veterinary sector, high-flow oxygen is revolutionising our care of dogs with severe hypoxaemia, which would otherwise have required mechanical ventilation. Sadly, this option remains non-viable for cats due to their very tiny nares, which are too small to accept the nasal prongs and minimally invasive oxygen therapy for cats remains centred around the use of an oxygen cage.
Looking to the future
The COVID-19 pandemic has generated renewed interest in producing affordable and portable ventilators, as well as less invasive forms of respiratory support. There is much we can still learn about how best to treat ARDS patients, without causing further injury to the lungs. Without a doubt, ongoing improvements in technology will enable us to further tailor respiratory support to individual patients, both furry and hairless alike, to maximise oxygenation and ventilation efficiency, whilst minimising VILI.
References
Brower RG et al. (2000). Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. New England Journal of Medicine 342(18), 1301–1308. https://doi.org/10.1056/ NEJM200005043421801.
Ceccherini G et al. (2020). Continuous positive airway pressure (CPAP) provision with a pediatric helmet for treatment of hypoxemic acute respiratory failure in dogs. Journal of Veterinary Emergency and Critical Care 30(1), 41–49. https://doi.org/10.1111/ vec.12920.
Fisher AB et al. (1984). Mechanisms of pulmonary oxygen toxicity. Lung 162(1), 255–259. https:// doi.org/10.1007/bf02715655.
Jagodich TA et al. 2020). High-flow nasal cannula oxygen therapy in acute hypoxemic respiratory failure in 22 dogs requiring oxygen support escalation. Journal of Veterinary Emergency and Critical Care 30(4), 364–375. https://doi.org/10.1111/ vec.12970.
Lumb AB (2017). Nunn’s Applied Respiratory Physiology Eighth Edition. Elsevier.
Plum F, Lukas DS (1951). An evaluation of the Cuirass respirator in acute poliomyelitis with respiratory insufficiency. American Journal of Medical Sciences, 221(4), 417–424. https://doi. org/10.1097/00000441-195104000-00009.
Shelhamer MC et al. (2020). Prone positioning in moderate to severe acute respiratory distress syndrome due to COVID-19: A cohort study and analysis of physiology. Journal of Intensive Care Medicine 36(2), 241–252. https://doi. org/10.1177/0885066620980399.
Sud S et al. (2014). Effect of prone positioning during mechanical ventilation on mortality among patients with acute respiratory distress syndrome: a systematic review and meta-analysis. Canadian Medical Association Journal 186(10), E381–E390. DOI: 10.1503/cmaj.140081.
Vassilev E, McMichael M (2004). An overview of positive pressure ventilation. Journal of Veterinary Emergency and Critical Care 14(1), 15–21. https:// doi.org/10.1111/j.1534-6935.2004.04002.
West JB (2008). Respiratory Physiology The Essentials Eighth Edition. Philadelphia: Lippincott Williams and Wilkins.
Woollam CHM (1976). The development of apparatus for negative pressure respiration (2) 1919 – 1976. Anaesthesia 31, 666–685. https://doi. org/10.1111/j.1365-2044.1976.tb11849.