Physiology News Magazine
Wanted – a time machine
Visual impairment increases with age. John Mellerio speculates as to why this is and requests a time machine to collect some easy answers.
Features
Wanted – a time machine
Visual impairment increases with age. John Mellerio speculates as to why this is and requests a time machine to collect some easy answers.
Features
John Mellerio
School of Biosciences, University of Westminster
https://doi.org/10.36866/pn.45.12

Life expectancy in 1900 was 45 years but in 2000 it was over 80. In 1951 there were fewer than 300 centenarians alive in the England and Wales: by 2035 it is estimated this number will be over 40,000. All this is, of course, a Good Thing. It came about because the diseases which killed off millions before their three score years and ten have largely been overcome. This success has allowed the so-called diseases of old age to enter the scene and now cancer, neurological problems, cardiovascular deterioration and various degenerations are the killers. And if people escape these, it seems they get senile and just wear out so they cannot resist a simple infection, like pneumonia, that a younger person would shake off.
Some people, noting that their motor cars work for longer and better if an effective program of preventative maintenance is carried out, have felt that it might be possible to take similar action with humans as they age. I am one of these people, but my expertise is in the limited area of vision. However, for the elderly, poor sight is an important disability and for the nation, a costly problem. It would be very worthwhile to come up with a life-time maintenance programme for vision and extend visual function to 100 years and more.
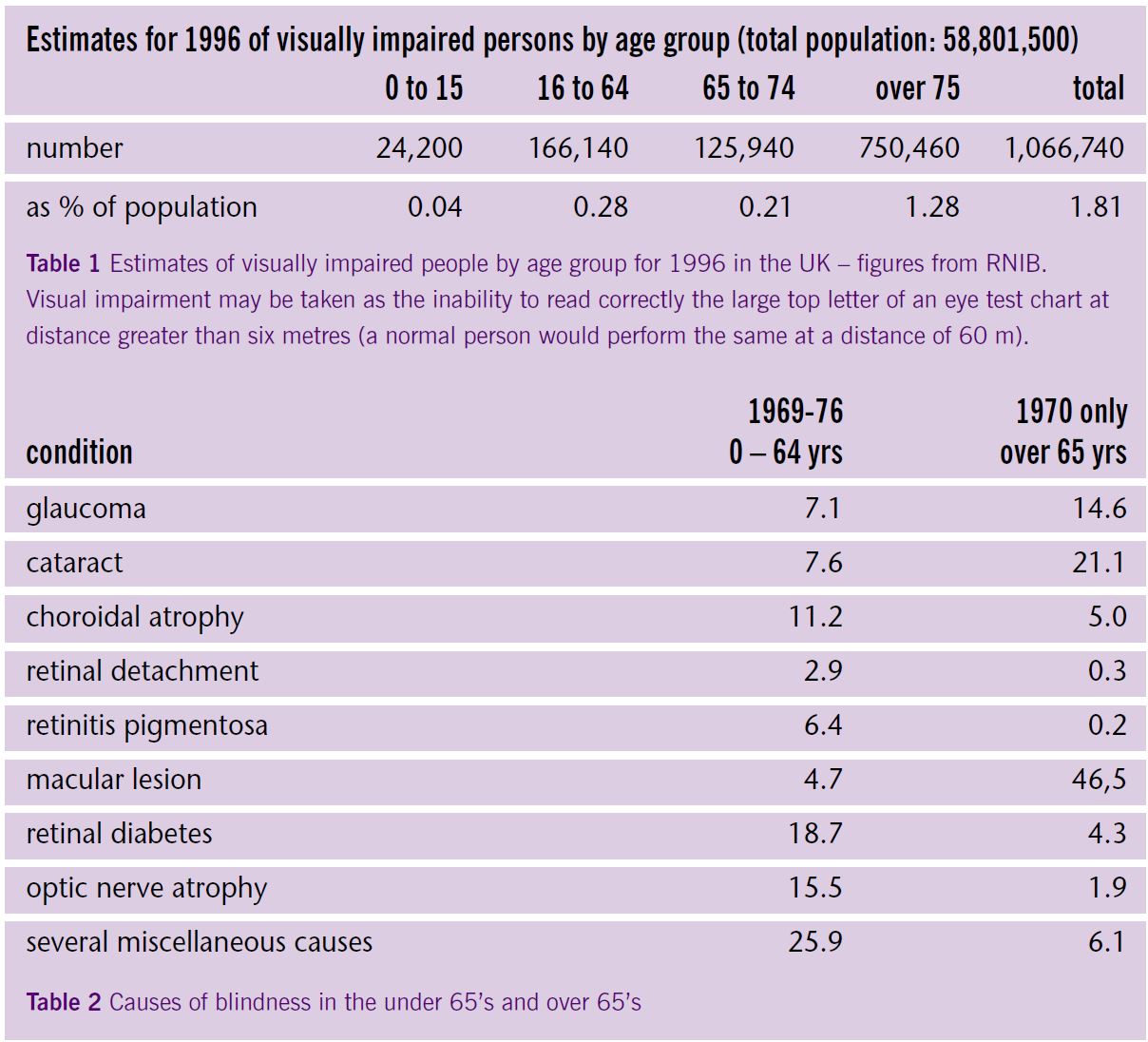
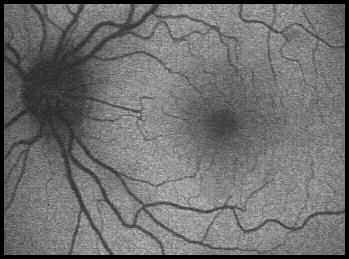
Table 1 shows how visually impaired numbers increase with age. The causes of visual impairment and blindness are many but they change with age as Table 2 shows. Below 65 years, diabetes and optic nerve atrophy are major causes, but for the over 65’s, macular lesions and cataracts head the list. These days cataracts are, in the developed world, no longer a serious problem and are easily removed, but macular lesions are a different story. Figures 1 & 2 show the retina at the back of the eye and how the foveal pit is positioned in the centre of the macula. Also shown is the position of the macular pigment (MP) within the retina. This pigment is a yellow mixture of two carotenoids, lutein (L) and zeaxanthin (Z). The presence of L and Z poses several questions, some of which we flatter ourselves by believing that we know the answer.
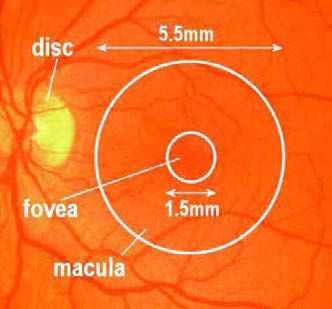
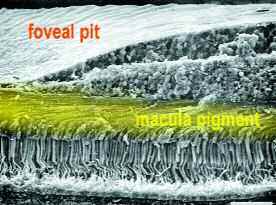
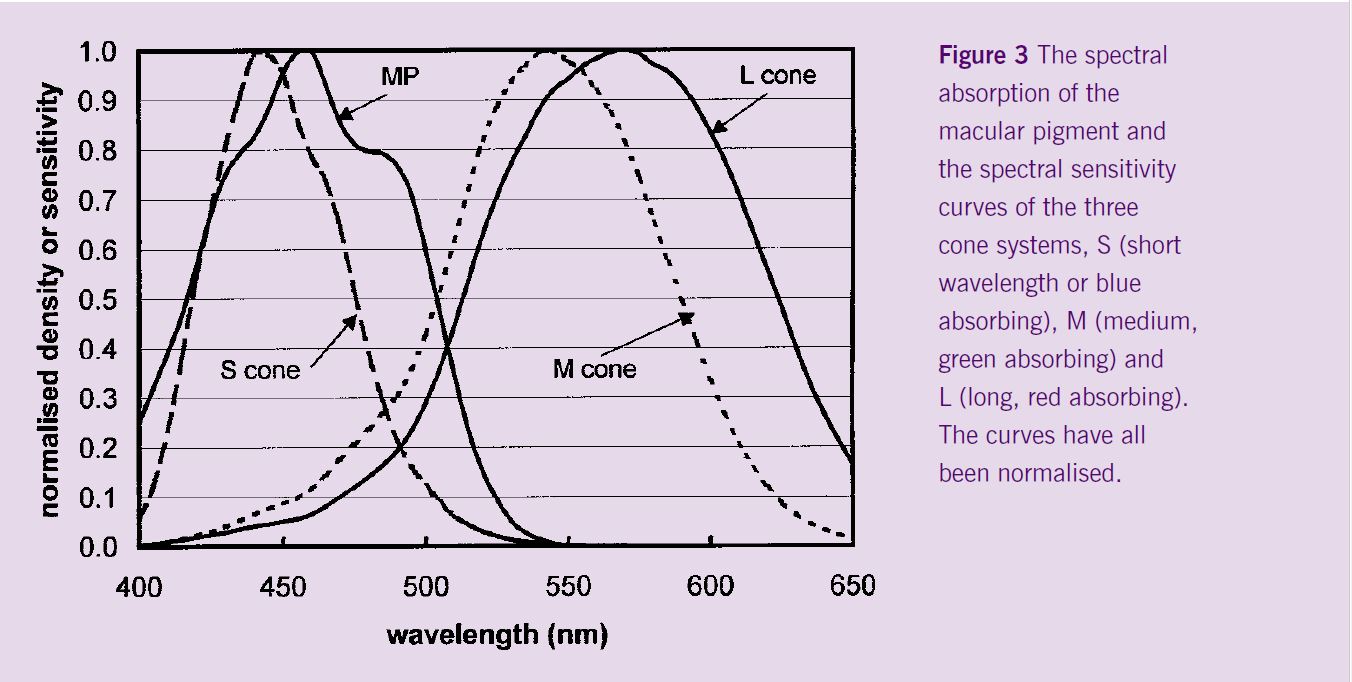
As Figure 2 shows, MP is situated in front of the light-sensitive outer segment portion of the photoreceptors which in the fovea are mostly cones. It is yellow which means that it absorbs blue light and this led to the first suggestion for the function of MP. The eye is not a perfect optical instrument, it suffers from chromatic aberration – the retinal image shows coloured fringes which will reduce the acuity of the eye. The yellow MP absorbs the blue light so the spread of the colour fringes will be reduced. Acting as a pre-receptor yellow filter, the MP would be expected to interfere with colour vision – indeed, the first attempts to measure the absorption spectrum and the amount of pigment present in an eye were made by vision scientists investigating colour vision. They wanted to know what the receptors would do without a yellow filter. Figure 3 shows that the spectral absorption curve for MP has a maximum absorption for blue light of 462 nm wavelength. Although the idea of MP as a chromatic aberration correcter is undoubtedly sound, it may not be very effective at this job (Hammond et al, 2001). On average, the optical density of MP is about 0.4 log units, i.e. it absorbs about 60% of the incident light, so some blue fringes would remain. Also, the centre of the fovea, the foveola where visual acuity is best, contains no blue sensitive or S cones which are responsible for absorbing blue short wavelength light to facilitate colour vision. It is as though the foveola is tritanopic, that is, it behaves as though it was blue colour blind. The MP will not, therefore, affect the blue channel of the trichromatic colour vision system at the very centre of gaze and its effect on the M and L cones (green and red absorbing, respectively) will be small, as Figure 3 shows. It remains to be shown how important for vision is the aberration correction function of MP.
MP, acting as a blue light absorber, has another role. It has been shown that short wavelength light, because of its relatively high photon energy, more readily damages the retina than yellow or red light which is less energetic. In animal experiments long exposures to levels of light such as are produced by fluorescent lamps or by a bright cloudy sky can lead to retinal damage and the short wavelength light is very effective in this. MP will absorb the energetic blue light and thus protect the photoreceptors of the macula. That MP is concentrated in the macula, around the optical axis of the eye, is an additional protective factor because the intensity of the retinal image is greatest in this on-axis area.
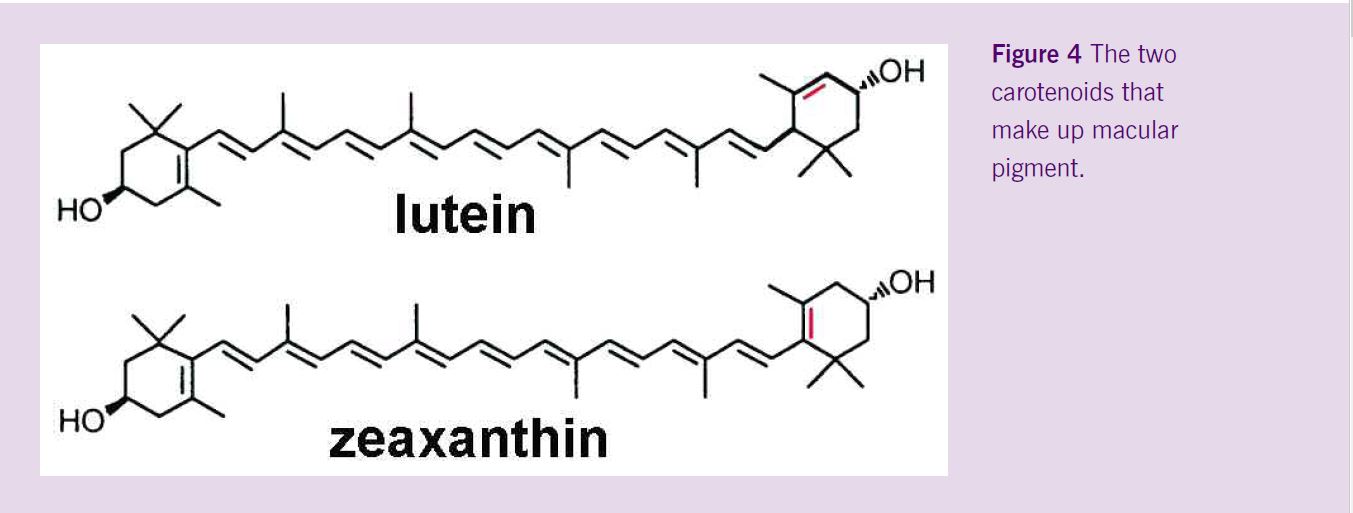
Recently, it has become apparent that MP has a much more important role in protecting the retina. Carotenoids in general are known for their antioxidant and free radical scavenging properties (Krinsky, 1989; Jacob & Burri, 1996). Lutein and zeaxanthin (Figure 4) are two very similar carotenoids that are not manufactured in the body but have to come directly from the diet. The best food sources of L and Z are not the same as for -carotine which is perhaps the most famous carotenoid. Whilst dark green vegetables (spinach and so on) were recommended as sources of L and Z, it seems that maize and orange pepper are better respectively for L and Z (Sommerberg et al 1998).
When radiation such as UV and short wavelength (blue) light interacts with tissues, especially with molecules called photosensitisers, there is formed a range of excited singlet state molecules. These are very reactive and are short lived: they lose the energy they gained in the excitation process by forming photoproducts, by fluorescing or by generating so-called triplet state molecules (Mellerio, 1991). These excited triplet state molecules are longer lived and may react with the molecules found in the tissues, especially with oxygen, to produce free radicals such as the oxygen free radical superoxide and the hydroxyl radical, or give rise to the destructive singlet oxygen. These various radicals are not good news as they can in turn oxidise tissue molecules. At especial risk are polyunsaturated fatty acids (PUFA) which enter a chain reaction called lipid peroxidation. Any cellular structure that is rich in PUFA’s is at risk, and the photosensitive outer segments of rods and cones are formed of stacks of discs made from plasma membrane rich in PUFA’s (Marshall, 1985). Figure 5 shows a rod outer segment in the first stages of light damage – the regularity of the discs is interrupted by centres of lipid peroxidation and the picture is reminiscent of a woolly sweater after a visitation by moths.

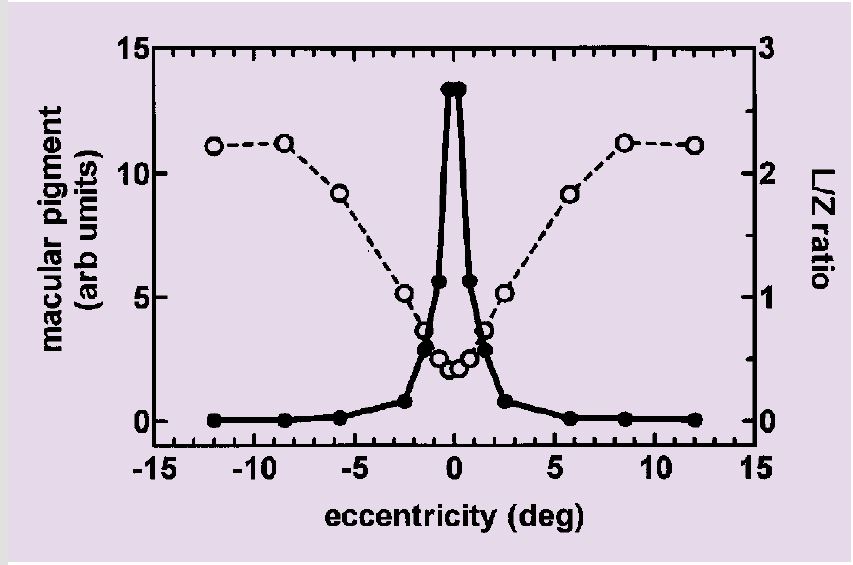
The two important protective properties of carotenoids, namely singlet oxygen quenching and the scavenging of reactive oxygen species, vary across the range of carotenoids and with the conditions used to measure these properties (Schalch et al, 1999). For example, in vitro, zeaxanthin has about twice the capacity to quench singlet oxygen of lutein and five times the ability to repair the -toco-pheryl radical cation. Whether these effectiveness ratios apply in vivo is not known, but it is interesting to see that L and Z are not equally distributed across the retina. In the fovea the ratio of L concentration to Z concentration is 0.7 and about 1.3 in the outer macular zone and higher still in the retinal periphery (Figure 6a). Indeed, L and Z occur in many retinal tissues but in much smaller amounts than in the fovea – free radicals are not only produced by the interaction of radiation and tissues, but are formed as byproducts of normal cellular metabolism, and all cells contain systems to mitigate against the destructive actions of these radicals.
The interest in the antioxidant properties of L and Z in MP arises because of laboratory experiments which show that prolonged exposure to light can induce damage to the retina and that the damage can resemble certain aspects of Age-related Macular Degeneration (AMD). Epidemiological research has suggested many factors that might predispose a person to AMD (Evans, 2001) but there is no universal consensus on all of these. One factor that the lab light-exposure experiments point to is chronic exposure to light, especially blue light and UV radiation. Oxidative stress is high in the retina, especially so in the fovea where the metabolic rate and the oxygen tensions are high, and where the incident light is most intense and there is a plethora of PUFA’S awaiting peroxidation (Beatty et al, 2000; Marshall, 1985). A good supply of carotenoid pigment in the macula would be a useful sight- preserving component to have throughout life to inhibit the slow destruction of the retinal cells. The idea that macular pigment is protective to retinal function (Haegerstrom-Portnoy, 1988) and AMD (Snodderly, 1995) is now firmly established but not at all confirmed.
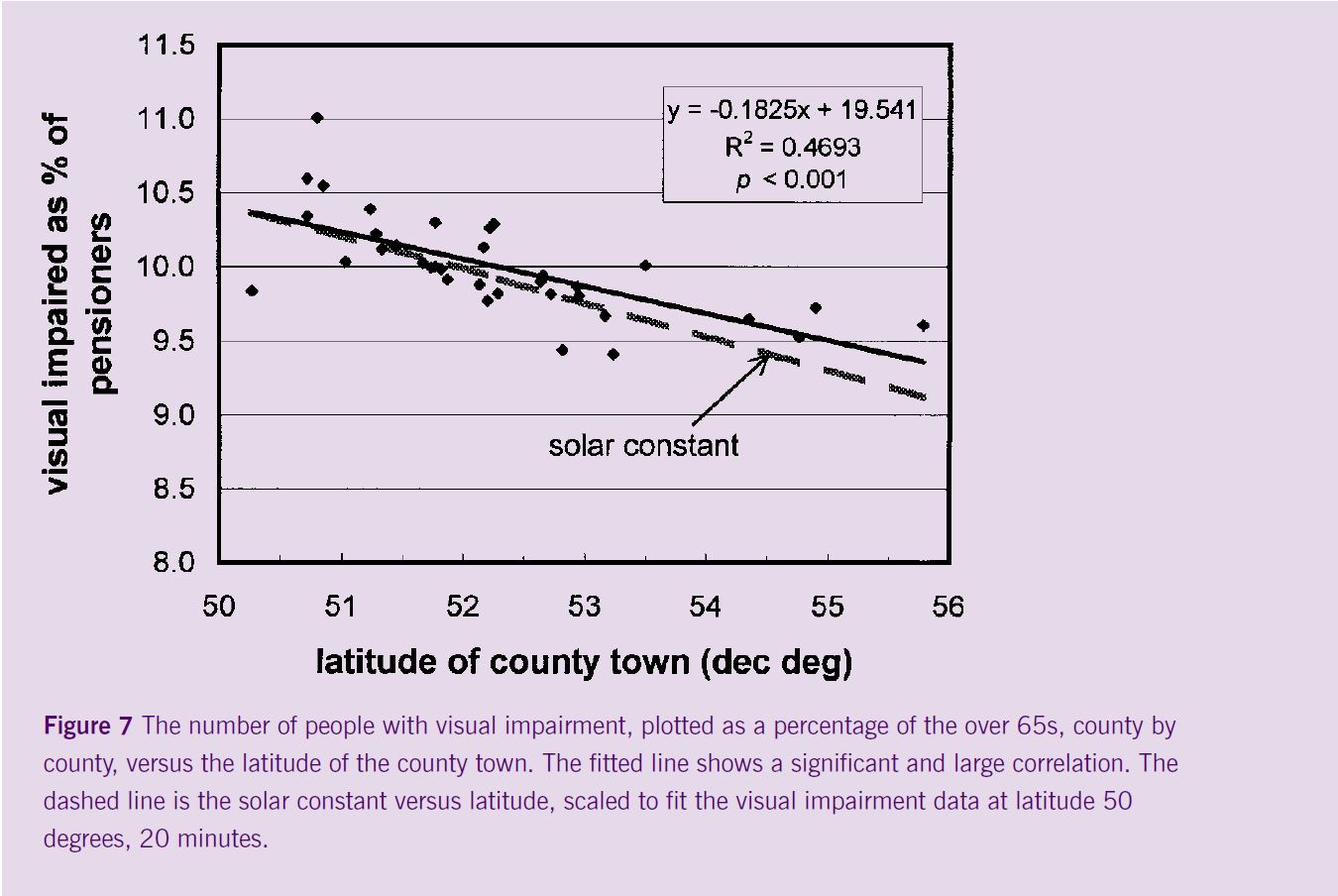
Although epidemiological studies (Taylor et al 1992; Cruickshanks, Klein & Klein, 1993) have shown that a history of exposure to strong sunlight is associated with an early onset of AMD, the effect is smaller than might be supposed from the very definite laboratory results that show that too much light of normal daylight intensity given over hours or days is harmful. However, associations between visual impairment and the amount of solar radiation in the subject’s locality may be seen even in the UK. Figure 7 plots, county by county, the percentage of visually impaired people (corrected for the size of the local cohort of elderly) against the latitude of the county town. The dashed line shows how the solar constant varies with latitude. These data are crude and open to criticism (the visual impaired figures include all impairing conditions and not just AMD), but they are suggestive and point up another good reason for living north of Potters Bar.
The situation for oxidative stress and light exposure in the eye is such that it might be sensible to err on the side of caution and, until it is proved otherwise, assume that there is a connection between light exposure history and AMD. Thus it would be worthwhile knowing if you have a high concentration of MP and, if not, to increase it. This would mean eating more L and Z in your diet – and, just as importantly, improving your life style by – yes, you guessed it – not smoking or drinking and keeping out of the sun, sun beds and tanning salons. MP levels can be measured fairly easily with small portable instruments that are just emerging from development (Mellerio et al, 1998; Wooten et al 1999) so screening is now possible.
Dietary intake of L and Z can be increased by eating more of the appropriate vegetables or by taking supplements. There are important questions about which supplement to take and how much, and whether this is safe and effective. A number of studies (Landrum, Bone and Kilburn, 1996) have shown increases in MP when the diet is supplemented with L but as L is mainly found outside the foveal centre (Figure 6), would supplementation with Z be better? So far only one pilot trial with Z supplementation has been reported (as poster at a meeting), but there is some evidence from elsewhere that L might be converted into Z in the fovea (Landrum and Bone, 2001). It was known that the distribution of MP across the macula, although radially symmetrical, may have wide or a narrow spread and this has recently been demonstrated nicely (Figure 6b) by van Kruijk et al (2001). It is an open question whether supplementation would widen the distribution or raise the peak value and what would be the best supplementation regime to achieve either or both effects.
Even though the ‘protection of MP against AMD’ theory is attractive, it needs to be proven. Beatty et al (2000) have measured MP values in AMD patients and shown they had less pigment than age matched normals, but the measurement is open to criticism. It was made using a psychophysical technique called heterochromatic flicker photometry which assumes that there are the same relative number of M and L cones in the fovea, where there is pigment, and outside at a comparison position where there is no pigment. In patients with AMD, this is not certain – indeed it is unlikely. And there is also the objection that it may not be low MP that leads to AMD – it may be that AMD causes so much retinal dysfunction that MP is lost and all that is measured is the progression of another facet of the disease. A similar relationship was found by Landrum et al (1999) when they measured MP levels in enucleated normal and AMD eyes by HPLC. But, as these authors state, an association does not necessarily reflect a causative relationship. The situation is complex and there are several confounding factors, e.g. age and race (Mare-Perlman et al 2001), to name just two.
What is required is a properly controlled longitudinal study that runs for about thirty years. Some of us with grey hair can’t wait that long, hence the need for a time machine to do in two years what nature would normally do in thirty. Does anyone know where I can get one?
References
Beatty S. Koh HH, Henson D, Boulton ME. The role of oxidative stress in the pathogenesis of age-related macular degeneration. Survey Ophthalm. 2000, 45:115-134.
Cruickshanks KJ, Klein R, Klein BE. Sunlight and age-related macular degeneration. The Beaver dam eye study. Arch Ophthalmol, 1993, 111:514-518.
Evans JR. Risk factors for age-related macular degeneration. Prog retinal Eye Res, 2001, 20:227-253.
Haegerstrom-Portnoy G. Short-wavelength-sensitive- cone sensitivity loss with aging: a protective role for macular pigment? Jnl Opt Soc Amer, 1988, 5:2140- 2144.
Hamond BR Jr, Wooten BR, Curran-Celentano J. Carotenoids in the retina and lens: possible acute and chronic effects on human visual performance. Arch Biochem Biophys, 2001, 385:41-46.
Jacob RA, Burri BJ. Oxidative damage and defense. Amer Jnl Clin Nutrition, 1996, 63: S985-S990.
Krinsky NI. Antioxidant functions of carotenoids. Free Radical Biol Med, 1989, 7:617-635.
Landrum JT, Bone RA. Lutein, zeaxanthin and the macular pigment. Arch Biochem Biophys, 2001, 385:28-40.
Landrum JT, Bone RA, Kilburn MD. The macular pigment: a possible role in protection from age- related macular degeneration. Adv. Pharmacol, 1996, 38:537-556.
Landrum IT, Bone RA, Chen Y, Herrero C, Llerena CM, Twarowska E. Carotenoids in the human retina. Pure Appl Chem, 1999, 71:2237-2244.
Mare-Perlman JA, Fisher M, Klein R, Palta M, Block G, Milieu AE, Wright JD. Lutein and zeaxanthin in the diet and serum, and their relation to age-related maculopathy in the third national health and nutrition examination study. Amer Jnl Epidemiol, 2001, 153:424-432.
Marshall J. Radiation and the aging eye. Ophthalmic Physiol Opt, 1985, 5:241-263
Mellerio J. The interaction of light with biological tissues and the potential for damage. In, Ed; Marshall J. The Susceptible Visual Apparatus, 1991, London, MacMillan Press, chapter 3.
Mellerio J. Interaction of Light on the Retina. In: Albert DM, Jakobiec FA. Principles and Practice of Ophthalmology: The Basis Sciences. 1994, Philadelphia, WB Saunders, chapter 116.
Mellerio J, Palmer DA, Rayner M.J. Macular Pigment Measurement with a Novel Portable Instrument (Abstract). Ophthalmic Res. 1998, 30 (suppL),302
Schalch W, Dayhaw-Barker P, Barker FM. The carotenoids of the human retina. In: Taylor A. Nutritional and Environmental Influences on the Eye, 1999, Boca Raton, CRC Press, chapter 12.
Sommerberg O, Keunen JE, Bird AC, van Kuijk FJ. Fruits and vegetables that are sources for lutein and zeaxanthin: the macular pigment in human eyes. Brit Jnl Ophthalmol, 1998, 82:907-910.
Snodderly DM. Evidence for protection against age- related macular degeneration by carotenoids and antioxidant vitamins. Amer Jnl Clin Nut. 1995,62:S1448-S1461.
Taylor HR, West S, Munoz B, Rosenthal FS, Bressler SB, Bressler NM. The long term effects of visible light on the eye. Arch Ophthalmol, 1992, 110:99-104.
Wooten BR, Hammond BR, Land RI, Snodderly DM. A practical method for measuring macular pigment optical density. Invest Ophthalmol Vis Sci. 1999, 40:2481-2489.
van Kruijk FJ, Pauleikhoff D, Fitzke F. Personal communication, 2001