How to rebuild the heart and muscle
Professor Georgina Ellison-Hughes, King’s College London, UK
“I love the challenge of trying to find ways to rebuild the heart and muscle,” says Professor Georgina Ellison-Hughes, a Professor of Regenerative Muscle Physiology at King’s College London, UK working on rejuvenating the heart’s reparative potential. Professor Ellison-Hughes tells us about her research and the detective work pursuing rarities residing in the adult heart that led to her career path in regenerative medicine.
“It’s not easy, and if I had spoken to my younger self knowing how challenging it is, maybe I wouldn’t have gone into this field!” Ellison-Hughes adds, “I love how my work feels like it could be in the realms of science fiction, especially when investigating how to reverse ageing and reprogramme cells back to healthy ones and even making ‘super’ cells”. She is excited to see how advancing and innovative technologies are turning the once sci fi elements of her work into a reality.

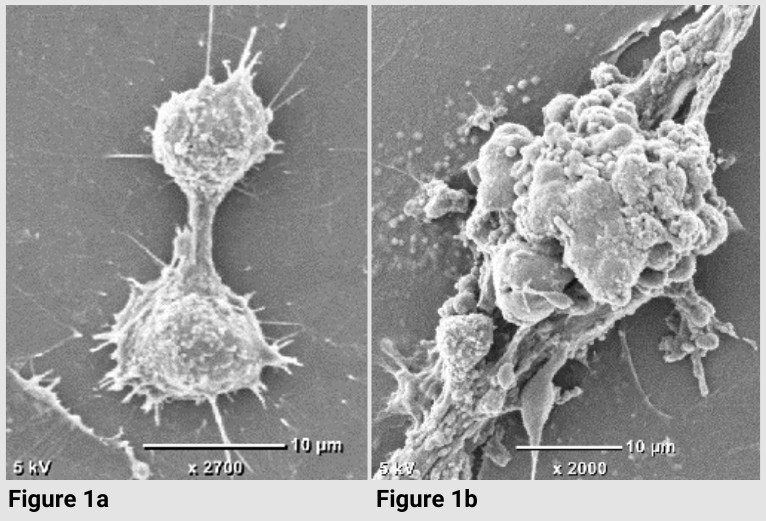
During my PhD, I investigated the ability of skeletal muscle to regenerate and form new muscle cells after injury. I was identifying small, immature, regenerating muscle fibres that expressed neonatal/embryonic major histocompatibility complex (MHC) cells. I worked on heart cross sections as my control, because at the time it was thought that no heart muscle cell regeneration or renewal took place in the adult heart. Except every time I carried out the immunostaining, I kept seeing these small, regenerating muscle cells in the heart. Not loads of them, just one or two per field of view.
Repair reserves
I explored the literature for answers. As I scrolled through papers, I found a group in America who had just published a paper showing these small, immature heart muscle cells in the adult human heart after injury (Beltrami et al., 2001). I thought that maybe I was seeing the same cells in my experiments. It just so happened that my PhD supervisor, Professor David F. Goldspink, knew one of the investigators on the paper, Dr Bernardo Nadal-Ginard, New York Medical College, US. My supervisor wrote to Dr Nadal-Ginard and told him about my findings. Next thing I knew, I was on a plane to New York, US, for a three-month lab visit to find out more about the regenerative capacity of the adult heart. That three months turned into four years. I graduated with my PhD and trained with some of the greatest scientific and inspiring minds to discover that the adult heart has a small, rare population of resident stem/progenitor cells that can give rise to new heart cells.
The heart, a self-renewing organ?
For the last few years, I’ve been working at the forefront of pioneering research on the heart’s capacity as a self-renewing organ. My research programme is focused on rejuvenating the regenerative capacity of striated (skeletal and cardiac) muscle, particularly preventing and treating the loss of muscle mass associated with ageing and/or disease. One way of doing this is to target cellular senescence.
This involves senotherapeutics, which are a class of therapeutic agents that target cellular senescence to help delay ageing and improve age-related diseases. I’ve been focused on senolytics in my research, which disable or eliminate senescent cells by inducing apoptosis.
Most of the heart failure patients that we aim to treat by regenerating their heart muscle are around 65 years and older. So, I focused my attention on what happens to the regenerative capacity of the heart with ageing. A few years ago, we showed that old age impairs the ability of the heart to repair and regenerate. And then using the senolytics, Dasatinib and Quercetin, we found that we can rejuvenate the heart’s reparative potential, where we see cardiac stem cell activation, new heart cell formation (Lewis-McDougall et al., 2019) and improved cardiac function (Zhu et al., 2015).
As well as working on how cellular senescence impairs heart regeneration and performance, and investigating the impact of different senotherapeutics to improve the heart’s regenerative potential, we are interested in combining senotherapeutics with cell therapy. This could improve the microenvironment, as well as the engraftment and survival of the transplanted cells.
Targeting cellular senescence
The difficulty with working on aged hearts and senescent cells is that they are incredibly delicate and stubborn. We must be really careful when doing experiments. Another tricky aspect is the on- and off-target effects of senotherapeutics, especially in the heart, which is such an important organ with a low cardiomyocyte renewal rate.
Clinical trials using senolytics to rejuvenate the heart’s reparative potential are already underway. They have reached phase I and II multi-centre trials with promising early results, showing an improvement in tissue, organ and physical function. Despite being a new class of anti-ageing drugs, we are seeing 2nd and 3rd generation senolytics coming through.
There are also approved agents that show senolytic properties, including the medicines, digoxin and SGLT2 inhibitors, which are used to treat heart conditions and lower blood glucose levels for people living with type 2 diabetes. In the next five years, senolytics could be part of clinical practice for treating a multiple range of age-related diseases, including cardiovascular disease, Type 2 diabetes and obesity.
Professor Georgina Ellison-Hughes will be presenting her research at The Biomedical Basis of Elite Performance 2024 on 19-20 December 2024. Taking part in the pharmacological interventions session, discussing ‘Can senotherapeutics rejuvenate muscle?’. Register now to hear more about Professor Georgina Ellison-Hughes’ work, human adaptation and performance at our two-day meeting.