
How to improve the heart health of an ageing population
Dr Matthew Lancaster, University of Leeds, UK
The human heart can stiffen as we age, reducing its function and predisposing it to problems. Loss of elasticity is not the only change that can compromise our heart. We interviewed Dr Matthew Lancaster (University of Leeds, UK) to learn more about what disrupts our heart’s functional capacity as we get older and what can be done to improve the heart health of an ageing population.
Dr Matthew Lancaster published the results of his Undergraduate BSc (Physiology) dissertation project in Experimental Physiology in the 90s. This early accomplishment in his career grew from a summer studentship, aided with a grant from The Physiological Society, to investigate metabolic inhibition and how the heart changes in response to ischemia (restricted blood flow). He is now Associate Professor in Exercise Physiology at University of Leeds, UK, an expert in cardiac ageing, arrhythmias and cardiovascular responses to exercise. Dr Lancaster loves to get stuck into any practical experiments in physiology, an enthusiasm that started early during his studies. It can lead to interesting discomfort though, including hypothermia such as experienced during cold-water immersion experiments testing if cardiovascular reflexes diminish in cold conditions. Such things don’t deter him but instead have continually spurred his interest to pursue different lines of physiological investigation. Throughout his career he has often tested himself, as well as using other models to find out more about the experimental processes and to learn what happens to the heart to understand how it responds to exercise and ageing.

Loss of elasticity as we age
A healthy heart is your body’s muscular pump driving the key transport system of your body. It should have the flexibility to fill with blood as easily but then contract down to deliver its contents to the arterial blood vessels quickly and efficiently. Unfortunately, as we age, the heart can stiffen. This increases the effort required to fill it with blood as well as eject it again, so rather than resembling blowing up an elastic balloon with your mouth, it becomes the equivalent of needing a foot-pump to fill a football with air. In the heart this is achieved by increasing the work done by the atria. Associating with this though are changes in the structure of the atria, the upper ‘priming’ chambers of the heart, which become enlarged to cope with the changing stress.
Changes in the function and structure of the heart seem to be a normal consequence of living longer. Dr Matthew Lancaster (University of Leeds, UK) is among the researchers who are working to understand such alterations in an ageing population. Today, older persons (aged 65 and above) are the world’s fastest growing age group. In 2018, older persons outnumbered children under the age of five for the first time in human history.
The gains we’re seeing in life expectancy can bring health challenges too. There are some diseases that predominately affect older people, with the heart being a primary target.
The mechanics of heart rate control
Lancaster has devoted his research career understanding what harms the ageing heart and what increases its sensitivity to injury in old age. Although, human biology nor physiology were top of his original career choices. “I was most commonly found with a screwdriver in my hand, taking something apart, as my PhD supervisor would have told you.” Lancaster refers to his love of engineering. After originally failing to get onto an apprenticeship engineering programme with the RAF, it was a family friend and biology teacher who persuaded Dr Lancaster to study biology alongside his preferred subjects, physics and maths, to be a balanced scientist. “I discovered I was quite fond of biology. But I’ve always maintained that my interest is in engineering and physics, which drives my curiosity for how things work.”
Lancaster’s engineering mind set and problem-solving approach have been at the core of his career and crucial for investigating the inner workings of the heart. He has explored the heart’s cellular and molecular physiology, studying potassium channels, atrial cells and cells in the heart’s pacemaker, the sinoatrial node, to understand how different regions of the heart are controlled and regulated. From studying the mechanics of how the organ pumps to monitoring the heart rate response to events, such as exercise.
“To build a complete picture of what is controlling the heart, we need to work through the entire spectrum. Going from the top range, where we use electrocardiography to monitor heart rate response during activities such as cycling or running, to drilling into the details at the bottom end, studying the cells and molecules, to then work back up again to understand how each dot connects.”
Ageing and deceleration of heart rate
This has led Lancaster to working with a broad range of subjects including athletes such as Alistair Brownlee, the British triathlete who has won two Olympic gold medals. He was studying the impact of training, seeing how it could influence the structure and size of the heart. If exercise could reshape the structure of the heart, what other factors could change it and how do humans adapt. “This question actually links limitations in athletes as well as what happens with ageing,” says Lancaster.
As we get older, our hearts generally get bigger. Despite the size increase, our heart loses the ability to accelerate to the same maximal beating rates it achieved when we were young. “We’re still not quite sure why our maximal heart rate drops as we get older, but projecting forward this can potentially significantly limit cardiac and overall function in old age” says Lancaster.
The deceleration reduces our physical capacity. Super fit athletes, who have unusually low resting heart rates of around 37 beats per minute that can quickly race all the way up to 200 beats per minute during exercise, show massive breadth for adaptation for physical capacity. As we age, our resting heart rate could be around 80 beats per minute, with a maximal heart rate of only around 110 beats per minute. So, there is little margin for the heart to adapt and respond to exercise. “This significantly decreases our cardiac output, which is why the body can struggle to respond to exercise stress as we age,” explains Lancaster. Along with this the stability of the rhythm of the heart can become compromised and the heart becomes prone to dysfunction. In some cases, this may mean older individuals require implantation of an artificial pacemaker to maintain a stable adequate rhythm to the heart beat.
Cardiac enlargement: Good and bad
The large heart often seen in older individuals can help ensure a good cardiac output even at low heart rates, maintaining our physical capacity just as many athletes have enlarged hearts enhancing their peak capacity. While a smaller heart could reduce our cardiac output and physical fitness. A downside though is that having a big heart tends to predispose humans to arrhythmias, which are irregularities in heart rate or rhythm. “So, a big heart is not necessarily a good solution for our health,” says Lancaster. Key areas of the heart impacted by exercise and age include the atria. “The atria must give an extra little push to try and make sure the ventricles are primed with blood. This helps to maintain normal heart function and a good cardiac output, meaning your heart supplies sufficient blood to your organs and muscles.” If the atria are put under strain though they become enlarged which is associated with an increased risk of arrhythmias, such as atrial fibrillation. A rapidly increasing clinical problem which develops most commonly in the elderly.
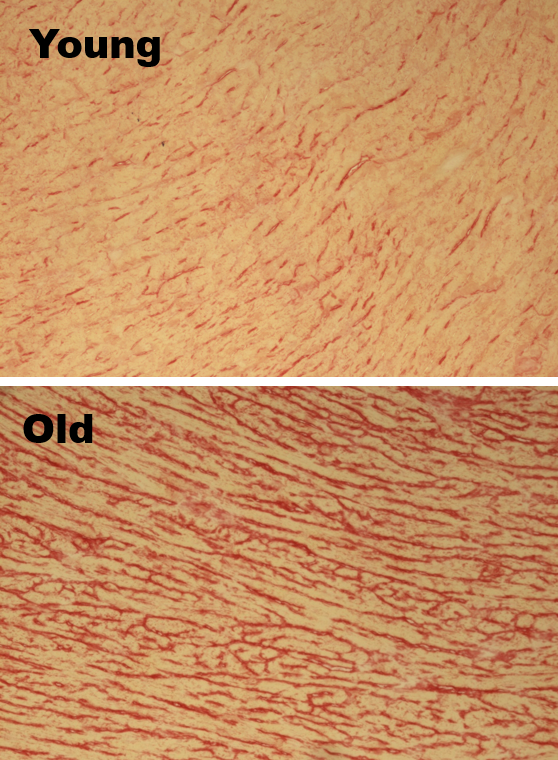
Figure 1. Collagen (stained red) content of the ventricle of the heart with age. The more you have the stiffer the heart is likely to be.
Scar tissue
Collagen, essentially the same material that forms a scar, for example when you slice your finger, usually serves a functional purpose in the heart, maintaining the tissue architecture and supporting the heart to coordinate its pumping action to drive blood into the body. The collagen is secreted by abundant key cells in the heart called cardiac fibroblasts. An enlarged heart is one normal response to stress on the system, but along with this can come inflammation and activation of cardiac fibroblasts. These will then secrete further collagen as a damage repair response, similar to the body’s response to repair a wound. The problem is that an increase in the density of the structural matrix of collagen is bad news for the heart. This impacts the efficiency of your body’s essential pump making it work harder. “The collagen stiffening the ventricles prevents them from relaxing as they should. This inability of the ventricles to fully relax, means that the upper chambers (the atria) must work harder,” explains Lancaster.
A common feature in the ageing population is a stiff heart, which disrupts how the heart contracts. In the last 20 years, there has been a rise in heart failure with preserved ejection fraction (HFpEF), a term more patients are hearing these days. HFpEF is a condition where the heart’s ability to fill with blood between heart beats, is hindered which reduces the amount of blood that the heart can then pump with each beat to circulate around the body. The origins of HFpEF may well lie in the accumulation of collagen in the heart over time and in response to stress. The question, says Lancaster, is how do we restore nice fluid healthy function in an aged and stiff heart? Ultimately, we need to break down the collagen or prevent accumulation to help people age healthily.

Figure 2. Former postdoc about to zap a heart being perfused to look at arrhythmia risk in the old heart.
Moderate workouts
The good news is that exercise can help with this. View it as an anti-inflammatory manoeuvre to protect your heart, and it turns out that moderation is best. “We’ve found that exercise can improve the body’s antioxidant capacity, almost acting as a shield from stress and damage.”
Lancaster tested this with mice running on treadmills for one year. The mice carried out modest exercise of 30 minutes running every other day. The activity didn’t get progressively faster or harder during the study, the idea was to maintain a steady and moderate exercise routine. It seemed to protect the ageing heart against the build-up of collagen deposition and preserved good heart function in the tested mice.
“It is a balancing act.” Lancaster explains: “Extreme exercise and frequent training at high intensity for long periods could potentially increase inflammation in the body. This could promote build-up of damaging levels of collagen and somewhat paradoxically increase the risk of arrhythmias, atrial fibrillation (an irregular and abnormally fast heart rate) and premature ageing.” Such exercise also promotes cardiac enlargement, a further risk factor for cardiac dysfunction.
Everything in moderation
Exercise doesn’t have to be elaborate or dramatic to have a meaningful effect, but it should be done regularly and throughout your life. Even a wall squat against a wall held for 30s up to a minute repeated regularly can lead to reduce blood pressure and so alleviate heart stress. “I’m afraid you can’t wait till you’re 70 to suddenly jump on the treadmill,” warns Lancaster. He carried out the treadmill study with aged mice, where introducing steady running late in life had no effect on improving the condition and function of their hearts. Only consistent physical activity was protective.
There remain challenges to solve on how best to protect our hearts as we age, with different reports and trials weighing in on the best forms of exercise, anti-inflammatory methods, and dietary interventions. Lancaster recommendation is to live a regular active lifestyle, alongside eating a Mediterranean diet with plenty of whole grains, fruit and vegetables. Hopefully, this could keep our hearts flexible, efficient, and protected from dysfunction to keep blood pumping healthily around the body even in old age.



